I found this article from 2001 during a bit of research - things haven't changed much.
Night shift: Six calls; one left at home; two by car; one by police van; two by ambulance.
Stats: 1 Dislocated elbow; 1 ? Drug overdose; 1 Chest pain; 2 EP fit; 1 eTOH.
One of the best dislocated elbows I’ve ever seen presented itself on my first call of the night after a 25 year-old Brazilian woman fell down the escalator at a tube station. Her heavy case fell and she tried to stop it but ended up following it down a few steps. Her arm did the job of stopping her vertical journey but it cost her the complete dislocation of her humerus from the radius and ulna so that it stuck out latero-posteriorly and looked like someone had just twisted it in an attempt to remove the lower arm. This type of dislocation is extremely rare.
Amazingly, she didn’t complain at all and told me it was ‘out of place’ when I examined her – yes, it was and the underground staff attending were amazed at the sight when I finally revealed it once layer upon layer of clothing had been carefully removed. She had a good distal pulse and a healthy capillary refill, so she went in the car, with a stable sling in place. Her routine will be x-ray, morphine and manual and probably aggressive reduction of the joint.
Oxford Street next for a 35 year-old female who apparently left a taxi to get money from a cashpoint but found herself without transport when the driver, who obviously got impatient or just didn’t like the look of her, threw her bags out and drove off. So, she collapsed in the street and MOPs gathered around her as she ‘behaved strangely’ - like she was having a fit.
A crew was with me when I arrived and I could see that, although she responded to pain, she was unwilling or unable to stay awake. Her pupils were tiny and her respirations were slow and shallow. On the ambulance she was given 800mcg of Narcan and her sleep continued, except when she had mini-fits of consciousness that made her flail around and lose bowel control.
She went to Resus and complained bitterly about having to take her top off, so she ran around the room making a nuisance of herself. Soon enough, I thought, she’ll fall down and go to sleep again.
At a train station a 49 year-old man had chest pain and a recent cardiac history with angioplasty, so when he told me he had unresolved pain despite GTN and aspirin, he got morphine to help. He threatened to collapse there and then but I think he was more anxious about the possibility of having a heart attack than the actual event taking place – his ECG said no but he went to hospital by ambulance.
After a break and a wasted journey out to a ‘vomiting with closing airway’, I got a call to an epileptic having a seizure. The crew arrived and together we headed up many, many flights of stairs – ignoring the lift for some strange reason - to the top floor, where we wheezed and panted as the 23 year-old woman’s mother explained that her daughter had been fitting irregularly and unpredictably recently and this latest episode worried her.
She was trying to sleep it off in bed when I rudely interrupted her rest and started my obs – she was looking normal except for a fast pulse, which is to be expected and then I handed over and left her to the crew so that a decision could be made about what should be done. She was left at home because I was still outside when the crew appeared patient-less and empty-chaired.
In the wee small hours a man was seen lying on the pavement ‘not moving’ and I went to check it out, asking that no ambulance be sent because the area I was heading to is notorious for this kind of sleeper – drink or drugs... or both. The police were on scene and two officers were helping the young man to his feet. Initially he was sluggish, sleepy and uncommunicative but a few minutes into the routine questioning carried out by the cops he reeled on one of them and was forcibly taken to a wall, pinned against it and handcuffed for his attitude.
I was about to put him into the car when this happened and of course I changed my mind. He would be travelling in a police van to hospital for what may or may not have been a drug-induced problem. On arrival, however, he sparked up and admitted to being a diagnosed depressive and drinker. ‘Why were you lying in the street?’ I asked. ‘That’s what I do’, he said.
He had been shopping and had a little bag containing tobacco, a can of soft drink and a can of dog food – hopefully for a dog and not himself. He was probably a waste of A&E time but it was quiet in the department and he hadn’t given the police an address to take him home to, so there really was no option. In the end I think he lied about his name and was generally cagey about where he lived because he just doesn’t like authority.
There’s nothing like causing a bit of trouble at 5.15 in the morning, so when a call for a ‘fit’ came in and I was sent to Horseguards I discovered that it was a soldier on the morning parade that had collapsed. Unfortunately, soldiers and horses were out in the dark, standing to attention amid the sounds of bugles and police motorcycles were controlling early traffic, including myself until I explained that I had to go in to attend this patient. Then I had to U-turn with an ambulance in tow, in front of the arriving royal car, stopping it in its tracks, to get through the gates and into the courtyard of Horseguards Parade.
We were ordered into a corner so that the royal dignitary could drive through on his way to inspect the soldiers and then a medic explained that he’d taken care of the patient and that it was nothing more than a stomach ache. An officer came over and introduced himself as the regimental doctor, saying much the same thing – the soldier was fine and we weren’t required. I have to say I felt very unwelcome and in the way. They’d already held up the parade because of us arriving, so I sensed they just wanted shot of us.
Once out of the area, I parked up to do the paperwork but another call came in about the soldier. This time I was to go around the back, to the parade ground itself. Police ushered me to a patrol car, inside which was seated a young Guardsman, in full uniform and great coat. He explained that he was epileptic and had fitted during the parade. He also told me that his medication was being ‘weaned’ off him. Now, I can’t understand this because epilepsy is something you can’t be weaned off – it’s not a bad habit. Having his drug cut in half meant he was bound to have a seizure as far as I’m concerned.
What struck me as emotive, however, was the story behind his condition. This tall 28-year-old Sergeant had been on patrol in Iraq when his squad was hit by an RPG, killing two of his comrades instantly, right in front of him. He sustained a head injury and this led to his epilepsy, which had been controlled by Epilim until now.
I found the whole thing worrying but, as an ex-army medic, I understood the politics of army life and sometimes things aren’t cut and dried. Sometimes you risk your life and get kicked in the face when you’ve survived.
He was an amiable man, very polite and determined to get on with his life – he has a plan for his family’s future and that’s something he can concentrate on while he copes with his condition.
Be safe.
Sunday 28 February 2010
Saturday 27 February 2010
Criminal offence
Night shift: Five calls; three declined; two by car. No ambulances tonight.
Stats: 1 Eye injury; 2 eTOH; 1 Head injury; 1 Vomiting.
I was told I looked a bit grey and unwell last night by a colleague. Maybe I’m working too hard.
We were short on ambulances tonight, like last night, so I was Control’s car-bitch and my first patient, who tripped and drunkenly fell onto her face outside a pub needed a short car journey to A&E more than an ambulance and crew anyway.
She had a huge swollen eye but the eyeball itself was in good order, although she couldn’t see from it due to the puffy, closed upper lid. She will be lucky to have escaped a fracture, judging by the severity of it. She was, as you can imagine, quite distressed about her injury and she wasn’t too drunk, so it was more of a lack of judgment that made her fall than an inability to stay upright. I drove her to A&E where friends met her and she chatted to them about her horrible night out.
I spent almost 4 hours of my shift giving a statement to the police as the result of the next call. My CRU colleague requested I convey a drunken 23 year-old man who was with his fiancé and a friend. He’d been celebrating his birthday but the alcohol had brought out the worst in him (or something else had) and he was verbally abusive from the start. Even then, I felt, with his fiancé on board, he could be taken home to sleep it off rather than into a crowded hospital where his language would cause concern. He spat expletives as if they were normal grammatical additions to conversation and I had to warn him many times about his behaviour towards me but he persisted in between strange calms.
At one point the door alarm on the car sounded and I realised that he had opened his door while I was moving. Normally the locks are on but I must have forgotten to engage this one and now he was attempting to get out of the car. I stopped and he stepped into the road, shouting as he did so. His behaviour was manic and bordering on psychotic.
I managed to get him back into the vehicle and continued the journey. I still had a duty of care and his fiancé, who’d been trying to quieten him down, was my concern too. For safety’s sake I requested that police meet us at his home address. Amid continued shouting and verbal abuse, some of which was extremely threatening towards me, he leaned forward and grabbed my shoulder, pulling me back into the seat. I disengaged his grip and warned him that the police had been called. Ironically, a police operation was taking place where I’d stopped and an officer asked if I was okay. I told him what had been going on and the man was promptly arrested.
This incident will no doubt cause the exponents against my role in conveying patients to say ‘we told you so’ but this risk is inherent in all patient transfers, in an ambulance or a car and his behaviour could not be measured accurately until it was too late. He didn’t become physically abusive until later and his language is something we all deal with on a regular basis. I agree that it may not be a risk worth taking and if his fiancé had not been with him I wouldn’t have carried him at all. Lesson learned though - next time, he/she or it will be thrown out of the vehicle.
On returning to my station a large piece of my car fell off and that put a damper on the night for me. Now I had a car off the road and it took me another two hours to get back on and only after ‘borrowing’ a vehicle from another department. Now the rest of my shift would involve ‘clearing up’ calls that were waiting, including a 30 year-old man who’d been assaulted – a girl had cracked a bottle over his head in a pub. He was an amiable young guy and he declined to go to hospital, so I checked him out and decided, as the bump on his head was almost three hours old, he may as well stay where he was.
This was swiftly followed by a call for a 22 year-old female who thought her drink had been spiked. The truth is, she was drunk. Her friends were with her and agreed to take her home to sleep it off after she declined to go to hospital.
Finally, as the rain-soaked battle mud settled in London I was sent to an 18 year-old man who was vomiting for the past 10 hours, apparently. His mother was with him and he did look rather pale but she wanted me to give him something as a quick fix because they were driving back home (a four hour trip) and she didn’t want him heaving up all over the car. Fair enough but at his age there was no quick fix and he was probably suffering a viral infection or had eaten something bad. Either way he was going to go through the vomiting motions until his brain got the message.
They didn’t fancy spending an eternity in A&E so I left them to sort it out with advice to call a GP or go to hospital if it continued.
* The stupid man who went for me in the car was fined and now has a criminal record.
Be safe.
Stats: 1 Eye injury; 2 eTOH; 1 Head injury; 1 Vomiting.
I was told I looked a bit grey and unwell last night by a colleague. Maybe I’m working too hard.
We were short on ambulances tonight, like last night, so I was Control’s car-bitch and my first patient, who tripped and drunkenly fell onto her face outside a pub needed a short car journey to A&E more than an ambulance and crew anyway.
She had a huge swollen eye but the eyeball itself was in good order, although she couldn’t see from it due to the puffy, closed upper lid. She will be lucky to have escaped a fracture, judging by the severity of it. She was, as you can imagine, quite distressed about her injury and she wasn’t too drunk, so it was more of a lack of judgment that made her fall than an inability to stay upright. I drove her to A&E where friends met her and she chatted to them about her horrible night out.
I spent almost 4 hours of my shift giving a statement to the police as the result of the next call. My CRU colleague requested I convey a drunken 23 year-old man who was with his fiancé and a friend. He’d been celebrating his birthday but the alcohol had brought out the worst in him (or something else had) and he was verbally abusive from the start. Even then, I felt, with his fiancé on board, he could be taken home to sleep it off rather than into a crowded hospital where his language would cause concern. He spat expletives as if they were normal grammatical additions to conversation and I had to warn him many times about his behaviour towards me but he persisted in between strange calms.
At one point the door alarm on the car sounded and I realised that he had opened his door while I was moving. Normally the locks are on but I must have forgotten to engage this one and now he was attempting to get out of the car. I stopped and he stepped into the road, shouting as he did so. His behaviour was manic and bordering on psychotic.
I managed to get him back into the vehicle and continued the journey. I still had a duty of care and his fiancé, who’d been trying to quieten him down, was my concern too. For safety’s sake I requested that police meet us at his home address. Amid continued shouting and verbal abuse, some of which was extremely threatening towards me, he leaned forward and grabbed my shoulder, pulling me back into the seat. I disengaged his grip and warned him that the police had been called. Ironically, a police operation was taking place where I’d stopped and an officer asked if I was okay. I told him what had been going on and the man was promptly arrested.
This incident will no doubt cause the exponents against my role in conveying patients to say ‘we told you so’ but this risk is inherent in all patient transfers, in an ambulance or a car and his behaviour could not be measured accurately until it was too late. He didn’t become physically abusive until later and his language is something we all deal with on a regular basis. I agree that it may not be a risk worth taking and if his fiancé had not been with him I wouldn’t have carried him at all. Lesson learned though - next time, he/she or it will be thrown out of the vehicle.
On returning to my station a large piece of my car fell off and that put a damper on the night for me. Now I had a car off the road and it took me another two hours to get back on and only after ‘borrowing’ a vehicle from another department. Now the rest of my shift would involve ‘clearing up’ calls that were waiting, including a 30 year-old man who’d been assaulted – a girl had cracked a bottle over his head in a pub. He was an amiable young guy and he declined to go to hospital, so I checked him out and decided, as the bump on his head was almost three hours old, he may as well stay where he was.
This was swiftly followed by a call for a 22 year-old female who thought her drink had been spiked. The truth is, she was drunk. Her friends were with her and agreed to take her home to sleep it off after she declined to go to hospital.
Finally, as the rain-soaked battle mud settled in London I was sent to an 18 year-old man who was vomiting for the past 10 hours, apparently. His mother was with him and he did look rather pale but she wanted me to give him something as a quick fix because they were driving back home (a four hour trip) and she didn’t want him heaving up all over the car. Fair enough but at his age there was no quick fix and he was probably suffering a viral infection or had eaten something bad. Either way he was going to go through the vomiting motions until his brain got the message.
They didn’t fancy spending an eternity in A&E so I left them to sort it out with advice to call a GP or go to hospital if it continued.
* The stupid man who went for me in the car was fined and now has a criminal record.
Be safe.
Friday 26 February 2010
Full moon madness
Night shift: Twelve calls; two declined; one assisted-only; three treated on scene; one by car; five by ambulance.
Stats: 2 Faints; 1 Fall (eTOH); 1 eTOH; 1 Chest pain; 3 Head injuries; 1 Hyperventilation; 1 Glass in foot; 1 Facial injuries (assault); 1 Blocked catheter.
I came in tonight and was told our HQ had been under attack from knife-wielding Gangsta-types who had spilled in through security during a fight which raged in the street. At least our Control colleagues got to see what we have to deal with out here at times.
A 71 year-old man collapsed in a theatre and this is not unusual in London’s old and very hot auditoriums – we get calls like this almost every day. This time, however, I was told he’d fainted twice before and although no cause had been identified after a barrage of medical tests, his pulse was too slow for his age (around 56bpm on average). His ECG and other readings were normal... it was just that slow pulse that bugged me.
I was sent an Urgent Care crew, despite asking them not to send anything yet until I’d checked the man out properly, and I used the opportunity to spend more time checking his vital signs and looking at his pulse rate to see if it would recover. After almost an hour with him, the rate hadn’t really changed much... it was nearer 60 than 50 but it still wasn’t right. He, however said he felt better and didn’t want to go to hospital, so after my usual three attempts, I gave up and he got a full report to take to his doctor on Monday.
I told him I was from Glasgow and he asked me the same standard question that everyone who is not from Glasgow asks... ‘are you Celtic or Rangers?’
Wolfe-Parkinson-White Syndrome can be fatal if not taken seriously, so my next patient, a 28 year-old woman suffering this condition who fainted in a restaurant got more of a priority response from me than she did from the staff who’d called after she fainted, recovered and felt like passing out again. Of course people faint all the time but here was a patient with a reason behind it and the possibility of deterioration or even sudden death, although unlikely.
I spent a while with her and her husband and got to know her history – she’d had two ablation treatments carried out and it’s possible they hadn’t been completely successful. It was equally possible that something else, something entirely benign, had made her faint. I wasn’t prepared to take the risk and I got her to hospital as soon as possible.
A fallen 49 year-old, who’d attracted the help of a few concerned MOPs, including a St. John Ambulance volunteer who just happened to be in the area, was drunk and nothing more. He reeked of booze and stale cigarettes but denied it of course. No wonder he fell on the pavement.
He had no injuries but got a Red response for a ‘head injury’ that didn’t exist. He got an ambulance of course.
Another non-runner who got an ambulance and a Red category was the 20 year-old man who fell asleep on the pavement at a bus stop. His can of Stella, which was rolling around him as he slumbered, was the give-away but it still didn’t stop the decent, honest, hard-working MOPs from dialling 999 and stating that he was ‘passed out’.
When I got there he was sitting up and the two female MOPs who’d called sheepishly informed me that he was 'awake now’. That I could see and further investigation revealed that he was also drunk, on drugs (‘I had a bit of weed’), on the streets and not interested in going to hospital. As interested in fact as the hospital would have been to receive him – they were extremely busy tonight.
So, after checking him out in the ambulance, I bundled him into my car, drove him to a quieter place, gave him a blanket and set him down in a doorway where I knew he wouldn’t be disturbed all night as he slept. He was very grateful.
One swiftly after the other when I am sent up to Charing Cross Road, which is already filling with ambulances and police for other incidents - for a 20 year-old man ‘having a heart attack’. An unlikely call given the nature of tonight’s Reds and this one joined the others as a wasted run. He was lying on the ground, with police officers and his mates around him. He was on anti-depressants and had a history of SVT but his pulse was regular and not at all tachy. He wouldn’t speak to me at first and had been the same with the police – this is not the behaviour of someone who is having a heart attack. He just didn’t want to talk.
The crew arrived as I was finally getting through to him and he told me he had chest pain, so of course that will be taken seriously now but he is known to the crew and they have had this from him before apparently.
Meanwhile, just up the road a man has fallen and now has a head injury and I’m asked on the radio if, when I’m free, I can go and attend to that call. I free myself up as soon as the crew have taken over with my chest pain man and walk up the 30 or so metres to the bar where the man fell. The police come with me because they haven’t received any calls about it and they’re curious. It’s also good protection for me because the crowd is getting ugly.
The man is sitting on a wall outside the bar and the doorman tells me he is okay and wants to go home. He has a minor cut to his forehead and is blind drunk, so no wonder he fell. I ask the man if he wants to go to hospital (guess how many times I ask) but he just wants a cab, so me and the two cops leave him to it.
A call to Leicester Square for a female who was having an asthma attack turned out to be a drunken woman who was hyperventilating and whose friends were frantically searching for a paper bag and had come up with a handful of dodgy newspaper from the pavement as an alternative. This call was routine and nothing at all but an ambulance trundled up and she was taken into the back of it to rest 'til she calmed down. While she did that, I was asked by a police officer to check on a girl at the north end of the square and I made my way up there to find a very, very drunken 19 year-old Bulgarian girl with her friends. She had fallen three times onto her head and now had a nasty swollen lump over her eye. Her mates swore that she didn’t drink but she was drunk on something because her behaviour was outrageous.
Head injuries can produce varying behaviour, including combativeness and I was very concerned that this young woman was in trouble. She certainly wasn’t coming with me in the car and her friends turned out to be a real handful too, as the cops around me struggled to keep them in line.
A fight broke out not far from me and a man turned up with a head injury and a cop in tow. His injuries looked severe enough to merit a trip to hospital and now I had this misbehaving Bulgarian girl and a recently beaten up 18 year-old man to deal with simultaneously. It was a tricky balance and I asked Control to send me two ambulances – an act I felt would have me condemned for the rest of the shift. Still, neither of them could travel with me and they couldn’t go together in the same vehicle.
The Bulgarian kicked off with a female police officer as she sat in my car waiting for the ambulance to arrive and had to be restrained a little, such was the madness of her attitude. Again, I think the head injury had a lot to do with that.
When the ambulances showed up, the head injuries were put in their appropriate place and I checked back on both. Hungarian girl had calmed down and thanked me with a long, tight hug and cheek kisses that were beginning to feel uncomfortable because I couldn’t break her grip (I must be getting old). The assaulted man now had thoracic spinal pain and I found a pattern bruise over the area of his back where he felt discomfort. Someone had put the boot in there (as they had done with his head), so he was collared and boarded. Doing the same with Bulgarian girl would have been impossible, even though she could have done with it as a precaution – she was far too feisty and I now knew that her hug-grip was Olympian, so there’d be no attempt at being silly.
As I cleared the paperwork for those calls, I received another and was on my way to a police station, inside which was a 29 year-old female and her boyfriend, along with two police officers. She’d been running away from someone who was threatening them after a bust-up outside a club and, in order to flee faster and more efficiently, she’d removed her high heeled shoes. This meant she was running barefoot and somehow she managed to run across broken glass in the street. What are the chances, eh?
As she gave her harrowing (ish) account of what had happened to the officer, I examined her foot – I gave it a good wipe down and then saw the problem – she had a sliver of glass embedded in the sole of her foot, right in the middle. I called off the ambulance and removed the offending glass while she winced and talked at the same time; quite a trick.
Now that the glass was out I checked the rest of her foot again and confirmed that all was well. But no, wait a minute, she still had some discomfort. When I pressed on the pad of her sole below the big toe, she said she felt something sharp inside the skin. I looked at it again and broke news to her that would probably embarrass her for a while to come. ‘That’s just a verucca’, I said... medically.
An alleged robbery-assault that resulted in a 29 year-old Irishman being beaten up and left with facial injuries, led me to the drizzly street where police were interviewing him and he was steadfastly refusing medical attention. I managed to befriend him enough to clean his wounds, which were minor to be honest, and he was passive enough, but when the officers asked him about who’d allegedly robbed him again he did something quite comical – he said ‘she took my wallet’. Now he’d been saying that a bunch of blokes had removed his wallet, taken nearly £500 in cash (do people really carry that much around on a night out?) and then thrown his credit card, and the empty wallet, back at him once he’d been soundly beaten.
‘She?’ said the very cynical police office who’d just asked me to travel back to the police station with him and an accompanying officer because they had no vehicles to do it.
‘Yeah, it was girl that robbed me’, he said unconvincingly.
I watched the police officer’s face harden and he turned to me and said, ‘I won’t take up any more of your time, thank you anyway’. That was code for ‘we are going to have another chat with this idiot, so you are free to take another call... something more important perhaps’. Then another fight started down the road and I got in my car and slunk away towards coffee if I could find it.
Later I was asked to ‘sign off’ an Urgent Care crew that was dealing with an 80 year-old man who’d fallen and cried out, causing a neighbour so much concern that she called an ambulance. The man’s daughter arrived and was able to explain that his urinal catheter hadn’t been changed for three months and so that was probably the problem. Sure enough, the old man was complaining of burning pain at the catheter site and a district nurse was called out to deal with it. I signed the PRF off and left them all to it....
...Until I went back to collect the ECG/defib they’d left behind.
Be safe.
Stats: 2 Faints; 1 Fall (eTOH); 1 eTOH; 1 Chest pain; 3 Head injuries; 1 Hyperventilation; 1 Glass in foot; 1 Facial injuries (assault); 1 Blocked catheter.
I came in tonight and was told our HQ had been under attack from knife-wielding Gangsta-types who had spilled in through security during a fight which raged in the street. At least our Control colleagues got to see what we have to deal with out here at times.
A 71 year-old man collapsed in a theatre and this is not unusual in London’s old and very hot auditoriums – we get calls like this almost every day. This time, however, I was told he’d fainted twice before and although no cause had been identified after a barrage of medical tests, his pulse was too slow for his age (around 56bpm on average). His ECG and other readings were normal... it was just that slow pulse that bugged me.
I was sent an Urgent Care crew, despite asking them not to send anything yet until I’d checked the man out properly, and I used the opportunity to spend more time checking his vital signs and looking at his pulse rate to see if it would recover. After almost an hour with him, the rate hadn’t really changed much... it was nearer 60 than 50 but it still wasn’t right. He, however said he felt better and didn’t want to go to hospital, so after my usual three attempts, I gave up and he got a full report to take to his doctor on Monday.
I told him I was from Glasgow and he asked me the same standard question that everyone who is not from Glasgow asks... ‘are you Celtic or Rangers?’
Wolfe-Parkinson-White Syndrome can be fatal if not taken seriously, so my next patient, a 28 year-old woman suffering this condition who fainted in a restaurant got more of a priority response from me than she did from the staff who’d called after she fainted, recovered and felt like passing out again. Of course people faint all the time but here was a patient with a reason behind it and the possibility of deterioration or even sudden death, although unlikely.
I spent a while with her and her husband and got to know her history – she’d had two ablation treatments carried out and it’s possible they hadn’t been completely successful. It was equally possible that something else, something entirely benign, had made her faint. I wasn’t prepared to take the risk and I got her to hospital as soon as possible.
A fallen 49 year-old, who’d attracted the help of a few concerned MOPs, including a St. John Ambulance volunteer who just happened to be in the area, was drunk and nothing more. He reeked of booze and stale cigarettes but denied it of course. No wonder he fell on the pavement.
He had no injuries but got a Red response for a ‘head injury’ that didn’t exist. He got an ambulance of course.
Another non-runner who got an ambulance and a Red category was the 20 year-old man who fell asleep on the pavement at a bus stop. His can of Stella, which was rolling around him as he slumbered, was the give-away but it still didn’t stop the decent, honest, hard-working MOPs from dialling 999 and stating that he was ‘passed out’.
When I got there he was sitting up and the two female MOPs who’d called sheepishly informed me that he was 'awake now’. That I could see and further investigation revealed that he was also drunk, on drugs (‘I had a bit of weed’), on the streets and not interested in going to hospital. As interested in fact as the hospital would have been to receive him – they were extremely busy tonight.
So, after checking him out in the ambulance, I bundled him into my car, drove him to a quieter place, gave him a blanket and set him down in a doorway where I knew he wouldn’t be disturbed all night as he slept. He was very grateful.
One swiftly after the other when I am sent up to Charing Cross Road, which is already filling with ambulances and police for other incidents - for a 20 year-old man ‘having a heart attack’. An unlikely call given the nature of tonight’s Reds and this one joined the others as a wasted run. He was lying on the ground, with police officers and his mates around him. He was on anti-depressants and had a history of SVT but his pulse was regular and not at all tachy. He wouldn’t speak to me at first and had been the same with the police – this is not the behaviour of someone who is having a heart attack. He just didn’t want to talk.
The crew arrived as I was finally getting through to him and he told me he had chest pain, so of course that will be taken seriously now but he is known to the crew and they have had this from him before apparently.
Meanwhile, just up the road a man has fallen and now has a head injury and I’m asked on the radio if, when I’m free, I can go and attend to that call. I free myself up as soon as the crew have taken over with my chest pain man and walk up the 30 or so metres to the bar where the man fell. The police come with me because they haven’t received any calls about it and they’re curious. It’s also good protection for me because the crowd is getting ugly.
The man is sitting on a wall outside the bar and the doorman tells me he is okay and wants to go home. He has a minor cut to his forehead and is blind drunk, so no wonder he fell. I ask the man if he wants to go to hospital (guess how many times I ask) but he just wants a cab, so me and the two cops leave him to it.
A call to Leicester Square for a female who was having an asthma attack turned out to be a drunken woman who was hyperventilating and whose friends were frantically searching for a paper bag and had come up with a handful of dodgy newspaper from the pavement as an alternative. This call was routine and nothing at all but an ambulance trundled up and she was taken into the back of it to rest 'til she calmed down. While she did that, I was asked by a police officer to check on a girl at the north end of the square and I made my way up there to find a very, very drunken 19 year-old Bulgarian girl with her friends. She had fallen three times onto her head and now had a nasty swollen lump over her eye. Her mates swore that she didn’t drink but she was drunk on something because her behaviour was outrageous.
Head injuries can produce varying behaviour, including combativeness and I was very concerned that this young woman was in trouble. She certainly wasn’t coming with me in the car and her friends turned out to be a real handful too, as the cops around me struggled to keep them in line.
A fight broke out not far from me and a man turned up with a head injury and a cop in tow. His injuries looked severe enough to merit a trip to hospital and now I had this misbehaving Bulgarian girl and a recently beaten up 18 year-old man to deal with simultaneously. It was a tricky balance and I asked Control to send me two ambulances – an act I felt would have me condemned for the rest of the shift. Still, neither of them could travel with me and they couldn’t go together in the same vehicle.
The Bulgarian kicked off with a female police officer as she sat in my car waiting for the ambulance to arrive and had to be restrained a little, such was the madness of her attitude. Again, I think the head injury had a lot to do with that.
When the ambulances showed up, the head injuries were put in their appropriate place and I checked back on both. Hungarian girl had calmed down and thanked me with a long, tight hug and cheek kisses that were beginning to feel uncomfortable because I couldn’t break her grip (I must be getting old). The assaulted man now had thoracic spinal pain and I found a pattern bruise over the area of his back where he felt discomfort. Someone had put the boot in there (as they had done with his head), so he was collared and boarded. Doing the same with Bulgarian girl would have been impossible, even though she could have done with it as a precaution – she was far too feisty and I now knew that her hug-grip was Olympian, so there’d be no attempt at being silly.
As I cleared the paperwork for those calls, I received another and was on my way to a police station, inside which was a 29 year-old female and her boyfriend, along with two police officers. She’d been running away from someone who was threatening them after a bust-up outside a club and, in order to flee faster and more efficiently, she’d removed her high heeled shoes. This meant she was running barefoot and somehow she managed to run across broken glass in the street. What are the chances, eh?
As she gave her harrowing (ish) account of what had happened to the officer, I examined her foot – I gave it a good wipe down and then saw the problem – she had a sliver of glass embedded in the sole of her foot, right in the middle. I called off the ambulance and removed the offending glass while she winced and talked at the same time; quite a trick.
Now that the glass was out I checked the rest of her foot again and confirmed that all was well. But no, wait a minute, she still had some discomfort. When I pressed on the pad of her sole below the big toe, she said she felt something sharp inside the skin. I looked at it again and broke news to her that would probably embarrass her for a while to come. ‘That’s just a verucca’, I said... medically.
An alleged robbery-assault that resulted in a 29 year-old Irishman being beaten up and left with facial injuries, led me to the drizzly street where police were interviewing him and he was steadfastly refusing medical attention. I managed to befriend him enough to clean his wounds, which were minor to be honest, and he was passive enough, but when the officers asked him about who’d allegedly robbed him again he did something quite comical – he said ‘she took my wallet’. Now he’d been saying that a bunch of blokes had removed his wallet, taken nearly £500 in cash (do people really carry that much around on a night out?) and then thrown his credit card, and the empty wallet, back at him once he’d been soundly beaten.
‘She?’ said the very cynical police office who’d just asked me to travel back to the police station with him and an accompanying officer because they had no vehicles to do it.
‘Yeah, it was girl that robbed me’, he said unconvincingly.
I watched the police officer’s face harden and he turned to me and said, ‘I won’t take up any more of your time, thank you anyway’. That was code for ‘we are going to have another chat with this idiot, so you are free to take another call... something more important perhaps’. Then another fight started down the road and I got in my car and slunk away towards coffee if I could find it.
Later I was asked to ‘sign off’ an Urgent Care crew that was dealing with an 80 year-old man who’d fallen and cried out, causing a neighbour so much concern that she called an ambulance. The man’s daughter arrived and was able to explain that his urinal catheter hadn’t been changed for three months and so that was probably the problem. Sure enough, the old man was complaining of burning pain at the catheter site and a district nurse was called out to deal with it. I signed the PRF off and left them all to it....
...Until I went back to collect the ECG/defib they’d left behind.
Be safe.
Thursday 25 February 2010
Red, red whine
Day shift: Seven calls; two assisted-only; three by car; two by ambulance.
Stats: 1 Back pain; 1 Palpitations; 1 Unwell alcoholic; 1 Lacerated hand; 1 Near faint and panic attack; 1 Faint; 1 Cut above eye.
The first call was a Red simply because the caller told us the patient was ‘not alert’. This is one of the vaguest and most confusing things to ask a MOP – ‘Is the patient alert?’ What kind of response do you really expect from most of the population, especially if they are not English-speaking? The 33 year-old man had slipped on a newly washed floor (the wet floor signs were up) and fallen onto his back, like that clumsy and obviously very blind woman on the TV claim-for-blame shark ad. He now had a tender coccyx (as you would) and the pain was radiating to his pelvis and upper leg. This is what happens when you land on it hard – it gets bruised.
The man was fit and well and there was no reason to believe he had anything more than a minor injury – yet it was given a Red2 on the basis of his ‘not alert’ status. And yes, I know, you can fracture your coccyx and it’s painful but it’s not life threatening. This category is reserved for immediately life-threatening or at least potentially-so calls. Even if ‘not alert’ in the absence of a head injury, would this be such a call? Does smashing you tail bones on a hard floor from standing constitute a near-death experience? Is the brain somehow directly connected to the tail?
This call became a resource-drain simply because the guy on the floor said things like ‘I can’t move my leg’ and ‘it’s really painful’. But he scored his pain at less than 5/10 and he stood and walked, with support. In fact, after a breakfast of Entonox, he declined his trip to hospital and hobbled right back into work. I’m just glad he’s tax payer.
Next, a 23 year-old described as having ‘chest pain’ was actually experiencing palpitations. She had a one-year history of Lupus (SLE), so any organ can be affected if she has a ‘flare’ and in this case, her heart seems to be involved. The disease is degenerative and if her heart is being affected adversely this is not a good thing for her future health.
She was stable enough when I arrived; no chest pain, just that fluttery feeling when your heart is racing. The crew arrived a few minutes after me and we took her out of the crowded and very noisy hotel reception (it’s a large tourist hotel...mainly for young people) and into the quiet ambulance for further tests and a trip to hospital.
As I ran to yet another Red call, this time for a 41 year-old Polish alcoholic resident at a hostel who was having ‘breathing problems’ that didn’t exist, I heard a call come in for a cardiac arrest. An 18-month-old child and another child had been involved in a road traffic incident. This is why we have the colour red in our system.
The man sat in his grotty, litter-decorated room, panting and puffing as if he’d just run a Marathon. He complained bitterly about not feeling well and being sick after telling me he hadn’t eaten for two days and had just been drinking cider and cheap white lightning. ‘Well, no wonder’, I said, suggesting the obvious but, as usual, there was no acceptance of a pre-written fate – no acknowledgement of something brought upon himself. It’s a disease they say. It’s a state of mind eventually, I say. Smoking can be beaten with determination and will-power and so can an addiction to alcohol – it’s all about what it’s worth to an individual to stop.
I took him to hospital myself and once in the back of the car his theatrical breathing stopped (not his breathing per se of course) and his ‘vomiting’, in which he’d been up-chucking gobs of plaster-looking phlegm into a small bucket (and sometimes out of his third floor window when the mood took him), ceased instantly, even though I had provided him with a perfectly good yellow clinical waste bag for his pretender-to-the-throne vomitus.
He was actually relaxed by the time we got to hospital and I’d like to think that my calming manner had influenced his mood but no, like almost all of these individuals, their purpose for going to hospital is to get into an environment where they can be ‘cured’ of any immediate problem that interferes with their drinking routine. On the way out of his room, he tried to light a cigarette – so his ‘breathing problem’ was of no significance to him as long as I was there because his attitude was pretty much that I would clean up any consequence for him.
On a building site, three storeys up where a hard hat is required if you want to keep your skull intact, a 55 year-old man was handling a hoisted RSJ when it got caught and then slid into his hand when it was freed. This heavy piece of steel sliced into the joint of his hand, at the point where the metacarpals meet the fingers, ripping it open and probably breaking the bone there. A cycle colleague was on scene and had already dressed the wound, which had stopped bleeding. I was asked to take him to hospital in the car, rather than an ambulance, which is fair enough.
He was a good-humoured man and the three of us managed to have a smile and a joke or two before I took him to A&E. The pain in his hand was bearable, he told me and he didn’t want analgesia for it – but then he didn’t know he would be waiting for two hours in hospital before being seen – poor bloke.
A Red call for a ? Stroke at a museum turned out to be a near-faint that converted into a panic attack with hyperventilation and clawed fingers (this occasionally happens). The whole ‘can’t feel my fingers’ triggered an emergency call for a suspected CVA but the lady was embarrassed by the fuss that had been caused and sat munching on a bread roll as I completed all the obs I needed to confirm that she didn’t need to go to hospital if she really didn’t want to. She got the usual three offer deal but, sensibly, declined.
Another patient who declined was the 85 year-old female who fainted for ‘ten minutes’ according to her friend. That to me is a wee bit more than a faint, which is generally defined as being less than a minute and I advised her to consider going to hospital. She was very strong-willed about seeing he GP rather than going into A&E and so I did all I could on scene as she recovered fully from her dark spell. Her ECG looked a little long and slow in the P-R interval department and her pulse stepped up in pace from slow to normal. Her BP remained lowish for her age (115 systolic) but she insisted this was normal for her and that she regularly played tennis to keep it that way (pulse and blood pressure of an ageing athlete then).
Before going to see this lady and her friends at a well-known restaurant, I had travelled to a train station for a man claiming back pain after admitting to having cirrhosis of the liver through drinking. He was already being attended to by a crew so I was redeployed for this patient. The call went from Red to Green in a short few seconds. When it’s red for an 85 year-old ‘collapsed’ that’s a genuine worry; when it goes green again, all things have to be considered.
So, she got to sign my PRF and she was given three opportunities to go to hospital. She seemed fine but I made her promise me she’d see her GP immediately. She told me she would but after her next scheduled tennis game.
My peddling friend (cycle paramedic) was given a call in Oxford Street and I sensed a perfect job for getting home on time. Sorry but sometimes it’s about finishing on time, unless someone’s life is at risk of course. In this case, a 50 year-old woman had walked into a glass door in a department store, cutting her eye and landing on her backside when she fell. She had a small laceration above her eye and hadn’t been knocked out... in fact, she had no other injury at all, so I drove up there, collected her and got her to A&E, with her husband, who had shown up in support, giving me ten minutes of paperwork and ‘filing’ to do before finishing my tour of earlies.
Next up... the dreaded weekend nights.
Be safe.
Stats: 1 Back pain; 1 Palpitations; 1 Unwell alcoholic; 1 Lacerated hand; 1 Near faint and panic attack; 1 Faint; 1 Cut above eye.
The first call was a Red simply because the caller told us the patient was ‘not alert’. This is one of the vaguest and most confusing things to ask a MOP – ‘Is the patient alert?’ What kind of response do you really expect from most of the population, especially if they are not English-speaking? The 33 year-old man had slipped on a newly washed floor (the wet floor signs were up) and fallen onto his back, like that clumsy and obviously very blind woman on the TV claim-for-blame shark ad. He now had a tender coccyx (as you would) and the pain was radiating to his pelvis and upper leg. This is what happens when you land on it hard – it gets bruised.
The man was fit and well and there was no reason to believe he had anything more than a minor injury – yet it was given a Red2 on the basis of his ‘not alert’ status. And yes, I know, you can fracture your coccyx and it’s painful but it’s not life threatening. This category is reserved for immediately life-threatening or at least potentially-so calls. Even if ‘not alert’ in the absence of a head injury, would this be such a call? Does smashing you tail bones on a hard floor from standing constitute a near-death experience? Is the brain somehow directly connected to the tail?
This call became a resource-drain simply because the guy on the floor said things like ‘I can’t move my leg’ and ‘it’s really painful’. But he scored his pain at less than 5/10 and he stood and walked, with support. In fact, after a breakfast of Entonox, he declined his trip to hospital and hobbled right back into work. I’m just glad he’s tax payer.
Next, a 23 year-old described as having ‘chest pain’ was actually experiencing palpitations. She had a one-year history of Lupus (SLE), so any organ can be affected if she has a ‘flare’ and in this case, her heart seems to be involved. The disease is degenerative and if her heart is being affected adversely this is not a good thing for her future health.
She was stable enough when I arrived; no chest pain, just that fluttery feeling when your heart is racing. The crew arrived a few minutes after me and we took her out of the crowded and very noisy hotel reception (it’s a large tourist hotel...mainly for young people) and into the quiet ambulance for further tests and a trip to hospital.
As I ran to yet another Red call, this time for a 41 year-old Polish alcoholic resident at a hostel who was having ‘breathing problems’ that didn’t exist, I heard a call come in for a cardiac arrest. An 18-month-old child and another child had been involved in a road traffic incident. This is why we have the colour red in our system.
The man sat in his grotty, litter-decorated room, panting and puffing as if he’d just run a Marathon. He complained bitterly about not feeling well and being sick after telling me he hadn’t eaten for two days and had just been drinking cider and cheap white lightning. ‘Well, no wonder’, I said, suggesting the obvious but, as usual, there was no acceptance of a pre-written fate – no acknowledgement of something brought upon himself. It’s a disease they say. It’s a state of mind eventually, I say. Smoking can be beaten with determination and will-power and so can an addiction to alcohol – it’s all about what it’s worth to an individual to stop.
I took him to hospital myself and once in the back of the car his theatrical breathing stopped (not his breathing per se of course) and his ‘vomiting’, in which he’d been up-chucking gobs of plaster-looking phlegm into a small bucket (and sometimes out of his third floor window when the mood took him), ceased instantly, even though I had provided him with a perfectly good yellow clinical waste bag for his pretender-to-the-throne vomitus.
He was actually relaxed by the time we got to hospital and I’d like to think that my calming manner had influenced his mood but no, like almost all of these individuals, their purpose for going to hospital is to get into an environment where they can be ‘cured’ of any immediate problem that interferes with their drinking routine. On the way out of his room, he tried to light a cigarette – so his ‘breathing problem’ was of no significance to him as long as I was there because his attitude was pretty much that I would clean up any consequence for him.
On a building site, three storeys up where a hard hat is required if you want to keep your skull intact, a 55 year-old man was handling a hoisted RSJ when it got caught and then slid into his hand when it was freed. This heavy piece of steel sliced into the joint of his hand, at the point where the metacarpals meet the fingers, ripping it open and probably breaking the bone there. A cycle colleague was on scene and had already dressed the wound, which had stopped bleeding. I was asked to take him to hospital in the car, rather than an ambulance, which is fair enough.
He was a good-humoured man and the three of us managed to have a smile and a joke or two before I took him to A&E. The pain in his hand was bearable, he told me and he didn’t want analgesia for it – but then he didn’t know he would be waiting for two hours in hospital before being seen – poor bloke.
A Red call for a ? Stroke at a museum turned out to be a near-faint that converted into a panic attack with hyperventilation and clawed fingers (this occasionally happens). The whole ‘can’t feel my fingers’ triggered an emergency call for a suspected CVA but the lady was embarrassed by the fuss that had been caused and sat munching on a bread roll as I completed all the obs I needed to confirm that she didn’t need to go to hospital if she really didn’t want to. She got the usual three offer deal but, sensibly, declined.
Another patient who declined was the 85 year-old female who fainted for ‘ten minutes’ according to her friend. That to me is a wee bit more than a faint, which is generally defined as being less than a minute and I advised her to consider going to hospital. She was very strong-willed about seeing he GP rather than going into A&E and so I did all I could on scene as she recovered fully from her dark spell. Her ECG looked a little long and slow in the P-R interval department and her pulse stepped up in pace from slow to normal. Her BP remained lowish for her age (115 systolic) but she insisted this was normal for her and that she regularly played tennis to keep it that way (pulse and blood pressure of an ageing athlete then).
Before going to see this lady and her friends at a well-known restaurant, I had travelled to a train station for a man claiming back pain after admitting to having cirrhosis of the liver through drinking. He was already being attended to by a crew so I was redeployed for this patient. The call went from Red to Green in a short few seconds. When it’s red for an 85 year-old ‘collapsed’ that’s a genuine worry; when it goes green again, all things have to be considered.
So, she got to sign my PRF and she was given three opportunities to go to hospital. She seemed fine but I made her promise me she’d see her GP immediately. She told me she would but after her next scheduled tennis game.
My peddling friend (cycle paramedic) was given a call in Oxford Street and I sensed a perfect job for getting home on time. Sorry but sometimes it’s about finishing on time, unless someone’s life is at risk of course. In this case, a 50 year-old woman had walked into a glass door in a department store, cutting her eye and landing on her backside when she fell. She had a small laceration above her eye and hadn’t been knocked out... in fact, she had no other injury at all, so I drove up there, collected her and got her to A&E, with her husband, who had shown up in support, giving me ten minutes of paperwork and ‘filing’ to do before finishing my tour of earlies.
Next up... the dreaded weekend nights.
Be safe.
Monday 22 February 2010
Assembly line medicine
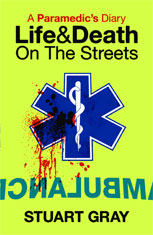
Probably the last thing you want to see after a hard-drinking 
night out.

night out.
Day shift: Six calls; five by car; one by ambulance.
Stats: 1 Chest pain; 2 Faints; 1 Back pain; 1 Numbness; 1 head injury.
A grey, rainy day today and the first call was for a chest pain in poshville, W1. The 77 year-old man woke up with tightness in his chest and his wife called an ambulance. The apartment was one of the nicest I’ve seen – very light and open with the usual private lift and concierge deal chucked in for a measly five million, or whatever these places cost nowadays. That place would be my post lottery-win London pad, that’s for sure.
Anyway, the crew was just ahead of me and I wasn’t required because the man was stable and there were enough hands to deal with him.
On the subject of Lottery wins – imagine winning fifty-odd million quid on Euromillions and earning £200,000 a month in interest. Imagine going to your bank manager (the new one of course ‘cos you’re not sticking with HSBC or Lloyds, are you?) and saying ‘right, I’ll leave my fifty-odd million in your bank but I need a ten million pound loan over ten years at a fair interest rate for you and I’ll use the interest I’m earning to pay off the loan in that time’.
Now, I’m no financier but I figured out that, after paying the interest every month, you’d still be looking at around £80,000 a month in earnings plus the benefit of buying all you needed with your ten million PLUS not laying a finger on your original winnings. Obviously, I hadn’t figured in the taxman... still nice fantasy. And of course someone is gonna come along and burst this bubble for me, right?
The day seemed to roll out fainters in excess because, as well as hearing my colleagues running to them I was sent to two in a row. The first was a 23 year-old female bank worker who collapsed on the floor of her open-plan office and began a charade that she had apparently gone through the previous year – same M.O. but no problem ever discovered for her behaviour. She vomited by means of forced retching until phlegm and mucus was deposited into a little plastic food container that someone had obviously contributed (after removing their sandwiches) and rolled around on the floor, giving periodical shaking displays as though fitting, when she clearly wasn’t. When I tried to sit her up, she threw herself back on the floor and when I tried to get her into a chair with wheels so that I could roll her, with the help of one of her male colleagues, out to the car, she deliberately slid off that too.
I asked for an ambulance because I’d had enough of struggling to make her behave but there were none to send and I spent a further fifteen minutes trying to convince her to help me out. All of her work colleagues could see what was happening and it doesn’t make good publicity for a reputation in such a closed environment.
After a long and unnecessary delay, during which she simultaneously went through her ‘seizure’ act and answered her colleague’s questions, I eventually got her to sit on that chair and we wheeled her out of the office, down in the lift and across the lobby floor to the exit, where she finally found the strength to stand up and walk to the car.
During the trip to hospital, she retched close to my ear whilst helping me to fill in the PRF details I needed. Strange but true.
Even stranger was the next fainter – a 50 year-old tourist woman from Italy. She was in a shoe shop when she collapsed and became unconscious for a short time, according to the staff. Obviously, whether she was unconscious or not is debatable and I asked her all the pertinent questions that might shed light on her sudden condition. She was very wide-eyed and confused and I have to say, a bit crazy looking – on drugs crazy... that type of look.
She initially declined my invitation to take her to hospital but changed her mind after I’d asked her for the third time (I always ask at least three times to be sure). She took my hand without it being offered and I walked her to the car. I would have had an ambulance take her to hospital, considering how confused she seemed to be but there was something naggingly familiar about her behaviour and I thought it would probably be best if I took her myself as it would only cost me 5 minutes.
All the way there I watched her in the rear view mirror and turned my head frequently to make sure I knew where she was. She sat behind the passenger seat – I never allow anyone to sit directly behind me when I am working alone. Usually if I have someone like Lottie out on Obs and she can keep an eye out for me I am much more able to relax but I had to keep tabs on her because I didn’t fancy having an ice-pick stuck into my neck. Okay, my imagination’s gone a little OTT.
After a break I was sent on a mission to recover a person who had fallen from a chair and now ‘could not move’. This sort of call deserves a quick investigation before sounding the bells because history has proven that they were notoriously stupid in nature and didn’t require an emergency ambulance in the first place – but what do you do when you have someone on the floor of your office and you have no first aider on duty, as stipulated by law? Tut, tut.
The 35 year-old Asian lady was like a jelly when I tried to examine her back – she did that pull away and wobble thing that you do when you anticipate pain but don’t actually experience it. She’d either fallen or launched herself off the chair (my money’s on launch) during a visit to a place that helps you find work in the UK if you are not from the UK; it’s a Government financed private business and you will have to forgive my sarcasm but it seems that we are paying taxes to fill the job market that is being created by redundancies and reluctance within the actual UK populace.
I got her to stand up and walk to the car, gave her a bit of entonox which helped and trundled her to hospital in the car. The ‘gas and air’ worked and she complained no more. Inside the A&E department it was chaotic – very busy indeed and a nurse had to announce that the waiting time had grown from two and half to three and a half hours. People were getting off buses in rows to go into the department. What was going on today? Outside in the ambulance parking area, there was an assembly-line of patients coming in, most of whom were in no way emergency cases
For example – a 21 year-old Romanian man who walked into a large department store with his suitcases (he’d just arrived in the UK) and told the staff he had numbness down one side. A Cycle responder was on scene after 999 was called. There was nothing wrong with him except for an emotional crisis at home but I was asked to taxi him to the nearest A&E dept, where he would cause a longer queue.
Then to finish the shift, one of my cycle colleagues gave me a last-minute job – a 4 year-old boy who’d tripped over and smacked his head in the street. He had a swollen eye and a little cut but was otherwise okay. We don’t like quiet children post-injury and he was a little too quiet after a head injury, so I put the lights and sirens on for a while and he sparked up and became a normal just-minor-injured little boy again. See? A little distraction works wonders in diffusing the worrying aspects of children’s illnesses and injuries. Try it before rushing to the phone to dial 999. Please.
A grey, rainy day today and the first call was for a chest pain in poshville, W1. The 77 year-old man woke up with tightness in his chest and his wife called an ambulance. The apartment was one of the nicest I’ve seen – very light and open with the usual private lift and concierge deal chucked in for a measly five million, or whatever these places cost nowadays. That place would be my post lottery-win London pad, that’s for sure.
Anyway, the crew was just ahead of me and I wasn’t required because the man was stable and there were enough hands to deal with him.
On the subject of Lottery wins – imagine winning fifty-odd million quid on Euromillions and earning £200,000 a month in interest. Imagine going to your bank manager (the new one of course ‘cos you’re not sticking with HSBC or Lloyds, are you?) and saying ‘right, I’ll leave my fifty-odd million in your bank but I need a ten million pound loan over ten years at a fair interest rate for you and I’ll use the interest I’m earning to pay off the loan in that time’.
Now, I’m no financier but I figured out that, after paying the interest every month, you’d still be looking at around £80,000 a month in earnings plus the benefit of buying all you needed with your ten million PLUS not laying a finger on your original winnings. Obviously, I hadn’t figured in the taxman... still nice fantasy. And of course someone is gonna come along and burst this bubble for me, right?
The day seemed to roll out fainters in excess because, as well as hearing my colleagues running to them I was sent to two in a row. The first was a 23 year-old female bank worker who collapsed on the floor of her open-plan office and began a charade that she had apparently gone through the previous year – same M.O. but no problem ever discovered for her behaviour. She vomited by means of forced retching until phlegm and mucus was deposited into a little plastic food container that someone had obviously contributed (after removing their sandwiches) and rolled around on the floor, giving periodical shaking displays as though fitting, when she clearly wasn’t. When I tried to sit her up, she threw herself back on the floor and when I tried to get her into a chair with wheels so that I could roll her, with the help of one of her male colleagues, out to the car, she deliberately slid off that too.
I asked for an ambulance because I’d had enough of struggling to make her behave but there were none to send and I spent a further fifteen minutes trying to convince her to help me out. All of her work colleagues could see what was happening and it doesn’t make good publicity for a reputation in such a closed environment.
After a long and unnecessary delay, during which she simultaneously went through her ‘seizure’ act and answered her colleague’s questions, I eventually got her to sit on that chair and we wheeled her out of the office, down in the lift and across the lobby floor to the exit, where she finally found the strength to stand up and walk to the car.
During the trip to hospital, she retched close to my ear whilst helping me to fill in the PRF details I needed. Strange but true.
Even stranger was the next fainter – a 50 year-old tourist woman from Italy. She was in a shoe shop when she collapsed and became unconscious for a short time, according to the staff. Obviously, whether she was unconscious or not is debatable and I asked her all the pertinent questions that might shed light on her sudden condition. She was very wide-eyed and confused and I have to say, a bit crazy looking – on drugs crazy... that type of look.
She initially declined my invitation to take her to hospital but changed her mind after I’d asked her for the third time (I always ask at least three times to be sure). She took my hand without it being offered and I walked her to the car. I would have had an ambulance take her to hospital, considering how confused she seemed to be but there was something naggingly familiar about her behaviour and I thought it would probably be best if I took her myself as it would only cost me 5 minutes.
All the way there I watched her in the rear view mirror and turned my head frequently to make sure I knew where she was. She sat behind the passenger seat – I never allow anyone to sit directly behind me when I am working alone. Usually if I have someone like Lottie out on Obs and she can keep an eye out for me I am much more able to relax but I had to keep tabs on her because I didn’t fancy having an ice-pick stuck into my neck. Okay, my imagination’s gone a little OTT.
After a break I was sent on a mission to recover a person who had fallen from a chair and now ‘could not move’. This sort of call deserves a quick investigation before sounding the bells because history has proven that they were notoriously stupid in nature and didn’t require an emergency ambulance in the first place – but what do you do when you have someone on the floor of your office and you have no first aider on duty, as stipulated by law? Tut, tut.
The 35 year-old Asian lady was like a jelly when I tried to examine her back – she did that pull away and wobble thing that you do when you anticipate pain but don’t actually experience it. She’d either fallen or launched herself off the chair (my money’s on launch) during a visit to a place that helps you find work in the UK if you are not from the UK; it’s a Government financed private business and you will have to forgive my sarcasm but it seems that we are paying taxes to fill the job market that is being created by redundancies and reluctance within the actual UK populace.
I got her to stand up and walk to the car, gave her a bit of entonox which helped and trundled her to hospital in the car. The ‘gas and air’ worked and she complained no more. Inside the A&E department it was chaotic – very busy indeed and a nurse had to announce that the waiting time had grown from two and half to three and a half hours. People were getting off buses in rows to go into the department. What was going on today? Outside in the ambulance parking area, there was an assembly-line of patients coming in, most of whom were in no way emergency cases
For example – a 21 year-old Romanian man who walked into a large department store with his suitcases (he’d just arrived in the UK) and told the staff he had numbness down one side. A Cycle responder was on scene after 999 was called. There was nothing wrong with him except for an emotional crisis at home but I was asked to taxi him to the nearest A&E dept, where he would cause a longer queue.
Then to finish the shift, one of my cycle colleagues gave me a last-minute job – a 4 year-old boy who’d tripped over and smacked his head in the street. He had a swollen eye and a little cut but was otherwise okay. We don’t like quiet children post-injury and he was a little too quiet after a head injury, so I put the lights and sirens on for a while and he sparked up and became a normal just-minor-injured little boy again. See? A little distraction works wonders in diffusing the worrying aspects of children’s illnesses and injuries. Try it before rushing to the phone to dial 999. Please.
Be safe.
Friday 19 February 2010
Balancing act
Day shift: Five calls; one refused; four by car.
Stats: 1 EP fit; 1 ? TIA; 1 ? fractured wrist; 1 eTOH; 1 Fractured foot.
During half-term holidays it takes about three hours for London to wake up and start calling ambulances in earnest, so it’s almost always slow for me first thing in the morning. This gives me the chance to wash the car, clean and replenish kit and generally catch up with stuff. At around 9am I can forget about these pauses.
A 20 year-old epileptic had a seizure at a train station and a passing doctor stopped to help. The doc was still with the patient when I arrived and I was given a handover that included a little bit of the history behind the fit. The young lady was very thin and very weak looking – vulnerable and fragile in appearance. She was emotional too and gripped my hand as I took a drop of blood for the BM test. I wondered if there was more to her condition than epilepsy.
When the crew arrived and the doctor left, she changed her mind about medical help and refused to go to hospital. So, she was allowed to get out of the ambulance and carry on with her journey – her health, her choice.
Another choice that had to be made was for the 38 year-old woman who was reportedly having a stroke at work. Her best friend and colleague had noticed slurred speech when she telephoned her after she failed to text in as normal before leaving for work, then when she arrived she seemed to have a facial droop accompanying her speech problem, so the friend dialled 999 and got me out to check.
With no medical history of any significance and a slightly high BP and recent stress in the background, I tried to persuade her to go to hospital by ambulance but she didn’t want to. Her facial droop was resolving and her FAST test arm weakness improved too but I was still convinced that she’d had a TIA and because it had probably happened within the past 6 hours, I wanted her to go directly to the appropriate unit for treatment, so I got her to agree to come with me (and her friend as company) in the car. She agreed to do that and was relaxed and happier for it I think. The journey took 5 minutes and she was seen by a doctor within one minute of arrival. In my book, that was a clinical decision that I had to take otherwise the choice was to drag her to an ambulance, causing further stress and upset... or leave her to make up her own mind with the possibility of another acute TIA or even a full blown stroke later on. These are not good options and so she went with me.
Barclays bank must be erring on the side of caution when it comes to promotion these days. Instead of TV advertising, they sent out four (soon to be out of work again) actors/singers/dancers, dressed in corporate blue costumes (a la marching band) around Soho to sing and dance while showing the bank’s logo prominently on a briefcase they each held. I know this because they stopped at my car as I waited on Frith Street, sipping a Latte, turned in unison, waved, gave me the thumbs up, mimed at me to smile (like banking with them is fun), made a ‘wind down your window’ gesture and then proceeded to sing and dance at me for 30 seconds before shutting down like robots, turning again as if on a parade ground and then stomping off in step (sort of) to unleash the same embarrassing ditty on someone else. Up and down the street they went. I thought I’d driven to Disneyworld by accident. Except in Disneyworld, apart from the prices, they don’t charge you interest and fees for showing up.
Fractures don’t figure highly on our list of priorities – not the common upper limb fractures anyway and so you can expect a Green-type response (in other words, we’ll get there when we can) while, quite possibly, some over-acting person lays on the floor rolling around reporting themselves to be ‘feeling faint’ and the ambulance is sent to him/her/it instead. You can sit on your own with a broken wrist, in quite some pain, while we run around after phantom emergencies. It’s a damned shame that we are driven to this on the basis of fear of getting it wrong and the blasé attitude of a computer coding system. A shame, therefore, that a perfectly lovely 75 year-old lady sat in a train station waiting to be taken to hospital for her (most likely) fractured wrist after she’d taken a tumble on the quite frankly ludicrous sloping surface of the walkway leading to the platform.
She was with her son and I got there a mere 9 minutes after the call was made and in this case all was well because I got her to X-Ray within 39 minutes of her fall, which isn’t bad considering what I have just said about the call category. This was entirely due to a human being looking at the call and deciding that, instead of sitting around on standby doing nothing, I could pop up the road and collect this lady for her inevitable trip to A&E. Otherwise, with our system and the demanding whim of some Londoners, she may well have sat there in the cold, not more than 300 meters from the hospital, for hours before being seen.
Yes, she could have walked or taken a taxi and I always bang on about this too but at that age, unsteady on her feet with pain and a history of high blood pressure, it’s reasonable to send someone like me trundling up to carry out the important clinical checks before things are made worse by moving her inappropriately and I always emphasize when teaching about fractures, the crucial element of pain and complications when deciding to go 999 on a relatively minor broken bone.
Her capillary refill was poor, indicating the fracture may be interfering with her radial circulation, so I made a slight adjustment to the angle of the wrist and placed it in a sling to keep it straight. This worked perfectly and I felt warm and fuzzy about having resolved that more significant issue. With blood now flowing properly to her hand (her thumb mainly), the bone could get on with being repaired by the experts... and her own body.
The police called to ask for assistance with a man who was ‘very drunk’ outside the Ritz (at least he had class). He’d been bothering people as they passed by and now he was just incapable of standing safely, so the officers wanted me to take him to hospital if possible. Now, this is a little tricky because he hadn’t been arrested and hadn’t been sectioned but he was drunk in a public place and a danger to himself if he fell down or walked into the busy road, so I agreed to take him to hospital (a place of safety) and, given that I was told he had a violent history, I asked for an officer to accompany him in the back. No ambulance was required and he was as gentle as a lamb, so no problem.
The female officer accompanied him in the car and her colleague drove behind us in the police vehicle. He had already given up a small bottle of amyl nitrate and confessed to being schizophrenic but whether he was telling the truth about his mental health or not was questionable. Nevertheless, he was going to hospital for assessment in case he’d taken in more than alcohol.
On the way there I was asked if I could take the police officers urgently to help a crew who were trying to deal with an aggressive patient. Other colleagues had gone in support of the ambulance crew at the scene but I had two cops with me and they would be needed, so I diverted and got there in less than 2 minutes. The patient was on a trolley bed, thrashing around and causing real problems for the crew. A few more pairs of hands helped out as motorcycle responders arrived and the two officers with me got into it.
Meanwhile my patient sat quietly in the back seat and I kept an eye on him. I wandered off for a few seconds and returned with the female police officer so that we could continue our original journey and when she got in the back, the patient was wearing her police hat. He’d been very amorous toward her in the car on the way in and had tried to hold her hand a few times, so I think he was getting serious about her with the whole hat thing going on.
After a short journey and an unnecessary dispute about whether he was in a place of safety, according to the law or not, I left to continue my shift. We’d been tied up on this single call for nearly two hours.
Then I had to make another rapid decision and risk egg on my face when I was tasked to deal with a 37 year-old man caught shoplifting who had injured his leg. It was out of my usual area but I wanted to help with this because there were no ambulances available.
When I arrived the police were on scene (and shop security staff) with a very irate man with a hugely swollen foot. I was shown a 20 foot wall and told he’d dropped from it onto the pavement below in a bid to escape. A quick calculation of mechanisms said he needed an ambulance but he had no other injury – no pain other than in his foot and he shouted repeatedly to be taken in the car to hospital because the pain was unbearable for him. With no ambulance available and my colleagues busy on other calls, I decided to take him, as he wished, in the car with, yet again, a police officer to accompany him. I got him in quickly and asked for the hospital to be alerted in case he needed to be seen by a specialist or in Resus but when I got to hospital they had taken it as a ‘blue call’.
His injury was isolated and non-life-threatening but the medics insisted they check him over just in case and I got no real problem from them about the decision to advise them of his arrival but it caused more of a fuss than it should have done and it left me feeling a little like my day was punching me in the face. So, I am thinking harder about my convey decisions. I still want to be able to function and save ambulances wherever possible but after today, it might be easier to pass the buck.
Be safe.
Stats: 1 EP fit; 1 ? TIA; 1 ? fractured wrist; 1 eTOH; 1 Fractured foot.
During half-term holidays it takes about three hours for London to wake up and start calling ambulances in earnest, so it’s almost always slow for me first thing in the morning. This gives me the chance to wash the car, clean and replenish kit and generally catch up with stuff. At around 9am I can forget about these pauses.
A 20 year-old epileptic had a seizure at a train station and a passing doctor stopped to help. The doc was still with the patient when I arrived and I was given a handover that included a little bit of the history behind the fit. The young lady was very thin and very weak looking – vulnerable and fragile in appearance. She was emotional too and gripped my hand as I took a drop of blood for the BM test. I wondered if there was more to her condition than epilepsy.
When the crew arrived and the doctor left, she changed her mind about medical help and refused to go to hospital. So, she was allowed to get out of the ambulance and carry on with her journey – her health, her choice.
Another choice that had to be made was for the 38 year-old woman who was reportedly having a stroke at work. Her best friend and colleague had noticed slurred speech when she telephoned her after she failed to text in as normal before leaving for work, then when she arrived she seemed to have a facial droop accompanying her speech problem, so the friend dialled 999 and got me out to check.
With no medical history of any significance and a slightly high BP and recent stress in the background, I tried to persuade her to go to hospital by ambulance but she didn’t want to. Her facial droop was resolving and her FAST test arm weakness improved too but I was still convinced that she’d had a TIA and because it had probably happened within the past 6 hours, I wanted her to go directly to the appropriate unit for treatment, so I got her to agree to come with me (and her friend as company) in the car. She agreed to do that and was relaxed and happier for it I think. The journey took 5 minutes and she was seen by a doctor within one minute of arrival. In my book, that was a clinical decision that I had to take otherwise the choice was to drag her to an ambulance, causing further stress and upset... or leave her to make up her own mind with the possibility of another acute TIA or even a full blown stroke later on. These are not good options and so she went with me.
Barclays bank must be erring on the side of caution when it comes to promotion these days. Instead of TV advertising, they sent out four (soon to be out of work again) actors/singers/dancers, dressed in corporate blue costumes (a la marching band) around Soho to sing and dance while showing the bank’s logo prominently on a briefcase they each held. I know this because they stopped at my car as I waited on Frith Street, sipping a Latte, turned in unison, waved, gave me the thumbs up, mimed at me to smile (like banking with them is fun), made a ‘wind down your window’ gesture and then proceeded to sing and dance at me for 30 seconds before shutting down like robots, turning again as if on a parade ground and then stomping off in step (sort of) to unleash the same embarrassing ditty on someone else. Up and down the street they went. I thought I’d driven to Disneyworld by accident. Except in Disneyworld, apart from the prices, they don’t charge you interest and fees for showing up.
Fractures don’t figure highly on our list of priorities – not the common upper limb fractures anyway and so you can expect a Green-type response (in other words, we’ll get there when we can) while, quite possibly, some over-acting person lays on the floor rolling around reporting themselves to be ‘feeling faint’ and the ambulance is sent to him/her/it instead. You can sit on your own with a broken wrist, in quite some pain, while we run around after phantom emergencies. It’s a damned shame that we are driven to this on the basis of fear of getting it wrong and the blasé attitude of a computer coding system. A shame, therefore, that a perfectly lovely 75 year-old lady sat in a train station waiting to be taken to hospital for her (most likely) fractured wrist after she’d taken a tumble on the quite frankly ludicrous sloping surface of the walkway leading to the platform.
She was with her son and I got there a mere 9 minutes after the call was made and in this case all was well because I got her to X-Ray within 39 minutes of her fall, which isn’t bad considering what I have just said about the call category. This was entirely due to a human being looking at the call and deciding that, instead of sitting around on standby doing nothing, I could pop up the road and collect this lady for her inevitable trip to A&E. Otherwise, with our system and the demanding whim of some Londoners, she may well have sat there in the cold, not more than 300 meters from the hospital, for hours before being seen.
Yes, she could have walked or taken a taxi and I always bang on about this too but at that age, unsteady on her feet with pain and a history of high blood pressure, it’s reasonable to send someone like me trundling up to carry out the important clinical checks before things are made worse by moving her inappropriately and I always emphasize when teaching about fractures, the crucial element of pain and complications when deciding to go 999 on a relatively minor broken bone.
Her capillary refill was poor, indicating the fracture may be interfering with her radial circulation, so I made a slight adjustment to the angle of the wrist and placed it in a sling to keep it straight. This worked perfectly and I felt warm and fuzzy about having resolved that more significant issue. With blood now flowing properly to her hand (her thumb mainly), the bone could get on with being repaired by the experts... and her own body.
The police called to ask for assistance with a man who was ‘very drunk’ outside the Ritz (at least he had class). He’d been bothering people as they passed by and now he was just incapable of standing safely, so the officers wanted me to take him to hospital if possible. Now, this is a little tricky because he hadn’t been arrested and hadn’t been sectioned but he was drunk in a public place and a danger to himself if he fell down or walked into the busy road, so I agreed to take him to hospital (a place of safety) and, given that I was told he had a violent history, I asked for an officer to accompany him in the back. No ambulance was required and he was as gentle as a lamb, so no problem.
The female officer accompanied him in the car and her colleague drove behind us in the police vehicle. He had already given up a small bottle of amyl nitrate and confessed to being schizophrenic but whether he was telling the truth about his mental health or not was questionable. Nevertheless, he was going to hospital for assessment in case he’d taken in more than alcohol.
On the way there I was asked if I could take the police officers urgently to help a crew who were trying to deal with an aggressive patient. Other colleagues had gone in support of the ambulance crew at the scene but I had two cops with me and they would be needed, so I diverted and got there in less than 2 minutes. The patient was on a trolley bed, thrashing around and causing real problems for the crew. A few more pairs of hands helped out as motorcycle responders arrived and the two officers with me got into it.
Meanwhile my patient sat quietly in the back seat and I kept an eye on him. I wandered off for a few seconds and returned with the female police officer so that we could continue our original journey and when she got in the back, the patient was wearing her police hat. He’d been very amorous toward her in the car on the way in and had tried to hold her hand a few times, so I think he was getting serious about her with the whole hat thing going on.
After a short journey and an unnecessary dispute about whether he was in a place of safety, according to the law or not, I left to continue my shift. We’d been tied up on this single call for nearly two hours.
Then I had to make another rapid decision and risk egg on my face when I was tasked to deal with a 37 year-old man caught shoplifting who had injured his leg. It was out of my usual area but I wanted to help with this because there were no ambulances available.
When I arrived the police were on scene (and shop security staff) with a very irate man with a hugely swollen foot. I was shown a 20 foot wall and told he’d dropped from it onto the pavement below in a bid to escape. A quick calculation of mechanisms said he needed an ambulance but he had no other injury – no pain other than in his foot and he shouted repeatedly to be taken in the car to hospital because the pain was unbearable for him. With no ambulance available and my colleagues busy on other calls, I decided to take him, as he wished, in the car with, yet again, a police officer to accompany him. I got him in quickly and asked for the hospital to be alerted in case he needed to be seen by a specialist or in Resus but when I got to hospital they had taken it as a ‘blue call’.
His injury was isolated and non-life-threatening but the medics insisted they check him over just in case and I got no real problem from them about the decision to advise them of his arrival but it caused more of a fuss than it should have done and it left me feeling a little like my day was punching me in the face. So, I am thinking harder about my convey decisions. I still want to be able to function and save ambulances wherever possible but after today, it might be easier to pass the buck.
Be safe.
Thursday 18 February 2010
Drunk and loaded
Day shift: Five calls; four by car, one by ambulance.
Stats: 1 Lacerated lip; 1 Asthma; 1 eTOH and vomiting; 1 eTOH and falling down.
I had the pleasure of hosting, on behalf of the Service, a paramedic from Yorkshire and so the first part of my shift was about tours and history and the usual rubbish I can ply people with when they are caught unawares. He was a thoroughly good chap and I enjoyed our chats, which mainly focussed on the differences between London’s ambulance service and his. He seemed suitably impressed with the way things are done down here, so I am hoping his report back home will be favourable. I'm also wondering what it is we are doing right.
So, first off – a 3 year-old boy, reported as being variably 8 years-old and 5 years-old, depending on who you spoke to, fell onto the back of his little sister’s buggy, splitting his lip open and puncturing a decent hole through it at the same time. The bleeding had stopped and his mum was quite happy to travel to hospital in the car (it was a three minute trip) rather than expose him to the further stress of an ambulance. He was bawling his eyes out and took some time to settle down but once in hospital, he seemed to calm.
A wasted trip later on for an unknown person who dialled 999 and proceeded to press the buttons on his phone rather than respond to the call-taker. It was either a hoax or an accidental call but either way, we had to check it out and an area search, that including the public toilets in Leicester Square, led to nothing.
A 23 year-old girl with asthma had an attack at work and one of my motorcycle colleagues was on scene dealing. He suggested that a trip to hospital in the car may be useful but when we got there, she’d pretty much fully recovered and was chatting away cheerily with him after agreeing to go and see her GP about it instead. I wasn’t needed but I spent the next 20 minutes or so chatting to her, her mum and her cheeky cousin, who worked in the same place. While my colleague continued his paperwork and my observer got cornered in conversation, I was privy to discussions about boyfriends who had no sense of direction when it came to faces and other amusing side-subjects. Sometimes the people I meet and interact with make this job a lot more fun - these three ladies did just that.
I left them to it after being offered cups of coffee and a job with a possible one million quid bonus.
Drunken street people shouldn’t carry large amounts of cash on them – for their own good. It was a mystery for me and the police officer who called us, to find a very inebriated, constantly vomiting 34 year-old alcoholic with a plaster cast on one leg, one shoe on and over a thousand pounds cash in his pocket. He wanted to go to hospital and said he had pancreatitis but he wasn’t complaining of abdominal pain – his vomit smelled of alcohol, so all he wanted was a bed, although he could easily afford to check in to any good hotel in London, he chose the 4-star L’hotel d’NHS instead. Rooms are free for a limited time (see the nurse for details).
Drunk number two fell onto the escalators at an underground station and cut his face. He probably broke his nose too; there was evidence of damage to it along the bridge. He’d been rescued by the staff after attempting to continue his travels by tube with a messy, bloody face and a drunken stagger. They caught up with him at a station near me and I was asked to look at him and decide whether or not he should travel. Obviously, he couldn’t and an ambulance arrived to take him away for his own safety.
He was a pleasant Spanish man who apologised every ten seconds for the trouble he was causing and in my book the very recognition of that fact makes it okay with me. So he got smiley Stu and a hand up the steps into the ambulance. Then he went and spoiled the moment by tripping up and once again falling onto his face in the ambulance as he took the last step inside – silly sausage (as they say in the old country... wherever sausages are famous... Germany probably).
Be safe.
Stats: 1 Lacerated lip; 1 Asthma; 1 eTOH and vomiting; 1 eTOH and falling down.
I had the pleasure of hosting, on behalf of the Service, a paramedic from Yorkshire and so the first part of my shift was about tours and history and the usual rubbish I can ply people with when they are caught unawares. He was a thoroughly good chap and I enjoyed our chats, which mainly focussed on the differences between London’s ambulance service and his. He seemed suitably impressed with the way things are done down here, so I am hoping his report back home will be favourable. I'm also wondering what it is we are doing right.
So, first off – a 3 year-old boy, reported as being variably 8 years-old and 5 years-old, depending on who you spoke to, fell onto the back of his little sister’s buggy, splitting his lip open and puncturing a decent hole through it at the same time. The bleeding had stopped and his mum was quite happy to travel to hospital in the car (it was a three minute trip) rather than expose him to the further stress of an ambulance. He was bawling his eyes out and took some time to settle down but once in hospital, he seemed to calm.
A wasted trip later on for an unknown person who dialled 999 and proceeded to press the buttons on his phone rather than respond to the call-taker. It was either a hoax or an accidental call but either way, we had to check it out and an area search, that including the public toilets in Leicester Square, led to nothing.
A 23 year-old girl with asthma had an attack at work and one of my motorcycle colleagues was on scene dealing. He suggested that a trip to hospital in the car may be useful but when we got there, she’d pretty much fully recovered and was chatting away cheerily with him after agreeing to go and see her GP about it instead. I wasn’t needed but I spent the next 20 minutes or so chatting to her, her mum and her cheeky cousin, who worked in the same place. While my colleague continued his paperwork and my observer got cornered in conversation, I was privy to discussions about boyfriends who had no sense of direction when it came to faces and other amusing side-subjects. Sometimes the people I meet and interact with make this job a lot more fun - these three ladies did just that.
I left them to it after being offered cups of coffee and a job with a possible one million quid bonus.
Drunken street people shouldn’t carry large amounts of cash on them – for their own good. It was a mystery for me and the police officer who called us, to find a very inebriated, constantly vomiting 34 year-old alcoholic with a plaster cast on one leg, one shoe on and over a thousand pounds cash in his pocket. He wanted to go to hospital and said he had pancreatitis but he wasn’t complaining of abdominal pain – his vomit smelled of alcohol, so all he wanted was a bed, although he could easily afford to check in to any good hotel in London, he chose the 4-star L’hotel d’NHS instead. Rooms are free for a limited time (see the nurse for details).
Drunk number two fell onto the escalators at an underground station and cut his face. He probably broke his nose too; there was evidence of damage to it along the bridge. He’d been rescued by the staff after attempting to continue his travels by tube with a messy, bloody face and a drunken stagger. They caught up with him at a station near me and I was asked to look at him and decide whether or not he should travel. Obviously, he couldn’t and an ambulance arrived to take him away for his own safety.
He was a pleasant Spanish man who apologised every ten seconds for the trouble he was causing and in my book the very recognition of that fact makes it okay with me. So he got smiley Stu and a hand up the steps into the ambulance. Then he went and spoiled the moment by tripping up and once again falling onto his face in the ambulance as he took the last step inside – silly sausage (as they say in the old country... wherever sausages are famous... Germany probably).
Be safe.
Wednesday 17 February 2010
Fly boy
 This is a Highland Cow - Hairy, horny and not very happy that I interrupted him while he was eating. A typical Scotsman!
This is a Highland Cow - Hairy, horny and not very happy that I interrupted him while he was eating. A typical Scotsman!I’m sitting in the departure lounge of Prestwick Airport, waiting to make my return flight after teaching a first aid course up here today but I am flying Ryanair and, as seems normal with these airlines (cheap as chips but not always reliable) my fellow passengers and I have been treated to a 4-hour delay, courtesy of a ‘technical problem’. These things happen I guess but I am on an early shift tomorrow and really needed to be home before dawn on the day I work! I therefore have time to add this to my blog because I haven’t been on duty for almost a week and it looks a bit threadbare.
Aficionados of Elvis will know that this little airport, near Kilmarnock in South Ayrshire, is famous because the King himself visited it whilst returning from his tour of duty for the US Army in 1960. The transport plane carrying him (and others obviously) landed to refuel as it travelled from Germany. This is supposed to be the only time that he ever stood on UK soil, although this was disputed by Tommy Steele who said he was in London with him during the 1950’s but that has never been proven and Prestwick jealously guards its historical claim with photographic evidence.
And because of that single visit to Scotland (when, on seeing the Scottish countryside the King is alleged to have said ‘where the f**k is this?’) – Prestwick has its own dedicated lounge and pictures of the great man are displayed around the terminal building. Bless. It is still one of the quietest airports I have ever flown to and from.
Going through security is a bit of fun too, isn’t it? We are all so used to having to remove our footwear that a little girl in front of me, who was no more than 8 years-old, deftly removed her softer than soft boots (nothing could be planted in them, even if you tried) and put them in the little basket for inspection. Then a wheelchair-bound man was asked to stand up (stand up, that’s right), to be searched when he came through the security gate, like he doesn’t have enough trouble and really wants to threaten everyone on the flight. We’ve gone a bit mad with this – we can’t be selective without being called racist and we can’t get a grip, so we are forced to go through this awful charade. All the while someone will be shouting in your ear ‘it’s for our own good. What if a plane blows up?’. Yes, there is a threat but there's dealing with it and there's being a paranoid, emotional wreck about it.
We could just make peace with people and stop irritating other nations to the point of hating us. We could butt out of the affairs of other ‘superpowers’ and get on with life – Switzerland isn’t currently being threatened with terrorism, is it? Or maybe that’s all a bit naive. Maybe reducing our liquids and gels to 100ml containers, all of which MUST be carried in a clear plastic bag, will radically cut the threat level. Has anyone even considered that as little as 100mls of any high explosive could do a good job of destroying a plane... or that having five bottles of liquids, masquerading as after shave, amounts to... hold on, I’m working it out... 500mls? Suddenly the volume of one container seems irrelevant and the whole idea stupid.
The rub is that if you get as far as the civilian security people, who hardly ever smile and are often just downright arrogant about their role, and you haven’t put your stuff into a clear plastic bag, they will take it away and bin it (you paid for it but now it’s gone) or, as in the case of Prestwick, point you in the direction of a handy machine, owned by the same company that makes those chewable toothbrushes, so that you can buy ‘security bags’ at £1 per 4. Twenty-five pence for a 2p plastic bag that calls itself a ‘security bag’ – is it any wonder people are being turned off the whole flying adventure?
To be fair, at Stansted, on my way out, I'd forgotten to remove toileteries from my hand luggage but, after a scan, search and rub down with explosive-detecting chemicals, the smiling (yep, friendly) security man gave me a plastic bag for them. See, getting on a plane can be a nice experience.
But then, inside the departure lounge, after all that security checking and plastic bag enclosing, they still put up signs advising you not to leave your bag unattended. Why the hell not? I’ve just been through a long and boring exercise with people who seem to judge me for the colour of my socks and now it’s still not safe to leave my bag alone for a few seconds? Is there something I should know?
Sometimes it’s good to get these things off my chest. I’m not very big on this whole authoritarian Government-led, terrorist-fed police state that we are entering into. Sure, we all need to be safe but safety is never guaranteed in life, however, being bullied and manipulated into thinking you need extra security is certainly guaranteed these days.
Xf
Wednesday 10 February 2010
Threats and laughs
Night shift: Five calls; one false alarm; four by car; none by ambulance.
Stats: 1 Alcoholic in pain; 1 Faint; 1 Head injury; 1 Sleeping person; 1 eTOH.
And here comes the snow again. It’s freezing out there and my second night with my Uni Student starts with a call to a less-than-beloved hostel for alcoholics and drug addicts. An abusive male has been calling for an ambulance on behalf of a female that is having chest pains, so it goes Red and I am sent to check it out because (and I don’t blame them) nobody on the desk is sure if this is a genuine call. When we arrive the staff has no idea what’s going on and we are shown up to the room where the call originated. That’s when the staff member decides to tell us that the guy inside has brandished a knife before and has a bit of a temper.
The door isn’t answered for nearly three minutes as we stand outside and the staff member shouts through it ‘Open up, the ambulance is here’. The man takes his sweet time to open up (remember this was a 999 call) and almost as soon as I step forward I am treated to verbal abuse and attitude. All I did was ask if the girl, who can clearly be seen in the room with another man, could put her cigarette out before we went in – that request sparked a spittle-loaded response.
I went in and asked what the problem was but the loud-mouthed man wouldn’t stop shouting and swearing, so it was difficult to get any sense out of the situation. The girl looked as if she was clucking for lack of booze or drugs, I didn’t know for sure which, and she was writhing around and yelling that her whole body hurt. She too became abusive after I informed them that I wasn’t going to take her anywhere under these circumstances. I needed them to calm down and let us do our job but this unleashed an even more personal and poisonous attack on me and I had noticed where his knife was, so I was keeping a corner of my eye on it. The student was behind me – this wasn’t really a suitable job for her to learn how to get attacked. We left the room to a rising melee of anti-Scottish, anti-ambulance abuse which had now been joined by the complete choir in the room and went back to the reception office with the staff member, who seemed embarrassed by this behaviour.
I asked for police and requested that no ambulance should be sent to this call. I knew the man upstairs would call 999 again and he did, several times. So we waited for the cops and when they arrived we all went back up and the two men were asked to leave the room so that we could assess the young woman who was in pain. The resident of the room, who had until then been fairly quiet, started shouting and swearing, telling us that he was not leaving his own room. Despite the fact that he was not this woman’s kin, he couldn’t see why she needed privacy during a clinical examination. But he caved in when I suggested the woman could walk out of the room instead (she’d told us that she couldn’t walk).
She was an alcoholic but denied taking drugs, even though she was a known Methadone user. Her body was a mess and the main problem affecting her health, which could never be fixed, was that her Liver was failing. She had generalised pain but it was the pain of a person who had inflicted it upon herself in a short lifetime of self-abuse. I will be surprised if she reaches the age of 30 - she's 23 now.
I can honestly say that this was one of the most menacing, threatening calls I've been on for a while and I would normally be working alone. This man was quite capable of taking that knife of his and sending me to the morgue. Why we, as a society, continue to put up with the evil that lives with us I will never know.
A 33 year-old American lady fainted outside a pub and we arrived to find her being tended by her husband and a few of the customers. Broken shards from a dropped glass lay around her as she recovered. She had a history of stomach problems but had never fainted before. We found her BP to be high, so we took her to hospital so that she could be assessed more thoroughly – rather that than miss something important. She was a very emotional person and I think this had a lot to do with current condition.
As the night ground into the late hours a 23 year-old woman fell down the stairs at an underground station and cracked her head on the floor when she landed. Her friend was with her and they’d both been drinking but not enough to be described as drunk. There was a good size bump on the crown of the falling girl’s head but she hadn’t been knocked out and she simply complained about how painful it was. It was a straight-forward transfer in the car – again because she’d been drinking, it was better safe than sorry.
A false alarm for a male ‘collapsed’ inside an office turned out to be one of the workers who’d decided to kip down on the floor for the night, either because he’d been drinking and couldn’t get home or because his wife had chucked him out. Whatever the reason, he was quite embarrassed when two police officers, the staff from an office above him and London Ambulance turned up.
Another embarrassed person; an Irish lady who fell onto her face and broke her tooth after being out with her daughter on a drinking marathon, will wake up in the morning and completely forget how she lost it. The ‘almost 50 year-old’ as she reminded me repeatedly, was conscious but unable to get up from the sitting position she’d been found in by PCSO’s when they arrived to help. Her daughter was a little worse for wear too and asked me to marry her a few times before finally understanding that I already was. They both went in the car and they kept us entertained all the way to hospital.
To be honest, I don’t mind a funny, well-meaning drunken person. I much prefer them to hard-nosed aggressive alcoholics or drug addicts who actually hate us because we spoil their party when it all goes wrong for them. This mother and daughter duo were funny and sincere. All the while the patient complained about losing a perfectly good tooth, her daughter laughed, like it was Ireland’s best joke. The young lady’s swearing was a bit too much to start with but I realised that was how she spoke and she meant no harm by it. I doubted the hospital staff could see that point of view on behalf of the other patients.
And the night ends with quite possibly the first slip and fall of the new day when a 40 year-old female slid on black ice at a crossing, falling onto her back. She was in some distress when we arrived and a MOP was taking care of her as best she could but a lot of the tears she was crying were in consequence of the event, rather than the pain I think.
My student almost came down just as hard when she too slipped on the treacherous surface as I tried to warn her. I had tested it when I got out of the car and what looked like surface water was in fact an ice rink – not funny for anyone and I could see how this day was going to develop unless the council got its act together and start gritting the pedestrian areas. We have only had a week’s warning about these conditions after all.
Be safe.
Stats: 1 Alcoholic in pain; 1 Faint; 1 Head injury; 1 Sleeping person; 1 eTOH.
And here comes the snow again. It’s freezing out there and my second night with my Uni Student starts with a call to a less-than-beloved hostel for alcoholics and drug addicts. An abusive male has been calling for an ambulance on behalf of a female that is having chest pains, so it goes Red and I am sent to check it out because (and I don’t blame them) nobody on the desk is sure if this is a genuine call. When we arrive the staff has no idea what’s going on and we are shown up to the room where the call originated. That’s when the staff member decides to tell us that the guy inside has brandished a knife before and has a bit of a temper.
The door isn’t answered for nearly three minutes as we stand outside and the staff member shouts through it ‘Open up, the ambulance is here’. The man takes his sweet time to open up (remember this was a 999 call) and almost as soon as I step forward I am treated to verbal abuse and attitude. All I did was ask if the girl, who can clearly be seen in the room with another man, could put her cigarette out before we went in – that request sparked a spittle-loaded response.
I went in and asked what the problem was but the loud-mouthed man wouldn’t stop shouting and swearing, so it was difficult to get any sense out of the situation. The girl looked as if she was clucking for lack of booze or drugs, I didn’t know for sure which, and she was writhing around and yelling that her whole body hurt. She too became abusive after I informed them that I wasn’t going to take her anywhere under these circumstances. I needed them to calm down and let us do our job but this unleashed an even more personal and poisonous attack on me and I had noticed where his knife was, so I was keeping a corner of my eye on it. The student was behind me – this wasn’t really a suitable job for her to learn how to get attacked. We left the room to a rising melee of anti-Scottish, anti-ambulance abuse which had now been joined by the complete choir in the room and went back to the reception office with the staff member, who seemed embarrassed by this behaviour.
I asked for police and requested that no ambulance should be sent to this call. I knew the man upstairs would call 999 again and he did, several times. So we waited for the cops and when they arrived we all went back up and the two men were asked to leave the room so that we could assess the young woman who was in pain. The resident of the room, who had until then been fairly quiet, started shouting and swearing, telling us that he was not leaving his own room. Despite the fact that he was not this woman’s kin, he couldn’t see why she needed privacy during a clinical examination. But he caved in when I suggested the woman could walk out of the room instead (she’d told us that she couldn’t walk).
She was an alcoholic but denied taking drugs, even though she was a known Methadone user. Her body was a mess and the main problem affecting her health, which could never be fixed, was that her Liver was failing. She had generalised pain but it was the pain of a person who had inflicted it upon herself in a short lifetime of self-abuse. I will be surprised if she reaches the age of 30 - she's 23 now.
I can honestly say that this was one of the most menacing, threatening calls I've been on for a while and I would normally be working alone. This man was quite capable of taking that knife of his and sending me to the morgue. Why we, as a society, continue to put up with the evil that lives with us I will never know.
A 33 year-old American lady fainted outside a pub and we arrived to find her being tended by her husband and a few of the customers. Broken shards from a dropped glass lay around her as she recovered. She had a history of stomach problems but had never fainted before. We found her BP to be high, so we took her to hospital so that she could be assessed more thoroughly – rather that than miss something important. She was a very emotional person and I think this had a lot to do with current condition.
As the night ground into the late hours a 23 year-old woman fell down the stairs at an underground station and cracked her head on the floor when she landed. Her friend was with her and they’d both been drinking but not enough to be described as drunk. There was a good size bump on the crown of the falling girl’s head but she hadn’t been knocked out and she simply complained about how painful it was. It was a straight-forward transfer in the car – again because she’d been drinking, it was better safe than sorry.
A false alarm for a male ‘collapsed’ inside an office turned out to be one of the workers who’d decided to kip down on the floor for the night, either because he’d been drinking and couldn’t get home or because his wife had chucked him out. Whatever the reason, he was quite embarrassed when two police officers, the staff from an office above him and London Ambulance turned up.
Another embarrassed person; an Irish lady who fell onto her face and broke her tooth after being out with her daughter on a drinking marathon, will wake up in the morning and completely forget how she lost it. The ‘almost 50 year-old’ as she reminded me repeatedly, was conscious but unable to get up from the sitting position she’d been found in by PCSO’s when they arrived to help. Her daughter was a little worse for wear too and asked me to marry her a few times before finally understanding that I already was. They both went in the car and they kept us entertained all the way to hospital.
To be honest, I don’t mind a funny, well-meaning drunken person. I much prefer them to hard-nosed aggressive alcoholics or drug addicts who actually hate us because we spoil their party when it all goes wrong for them. This mother and daughter duo were funny and sincere. All the while the patient complained about losing a perfectly good tooth, her daughter laughed, like it was Ireland’s best joke. The young lady’s swearing was a bit too much to start with but I realised that was how she spoke and she meant no harm by it. I doubted the hospital staff could see that point of view on behalf of the other patients.
And the night ends with quite possibly the first slip and fall of the new day when a 40 year-old female slid on black ice at a crossing, falling onto her back. She was in some distress when we arrived and a MOP was taking care of her as best she could but a lot of the tears she was crying were in consequence of the event, rather than the pain I think.
My student almost came down just as hard when she too slipped on the treacherous surface as I tried to warn her. I had tested it when I got out of the car and what looked like surface water was in fact an ice rink – not funny for anyone and I could see how this day was going to develop unless the council got its act together and start gritting the pedestrian areas. We have only had a week’s warning about these conditions after all.
Be safe.
Tuesday 9 February 2010
Adjustments
Night shift: Four calls; two declined; one by car; one by ambulance.
Stats: 2 Assaults; 1 eTOH; 1 Epistaxis.
I have a couple of nights with my student paramedic on board and before we’d even got a proper job, a man ran at the car in Soho and complained that he’d been assaulted and that we should treat him and call the police. He was a bit wild-eyed and edgy, so I called for police and watched as my student attempted to deal with his childishly minor injury, caused by a punch to the mouth. He got predictably annoying and aggressive and so I asked him to go and that the police would deal with it.
By the time the cops arrived on foot he’d long gone and the people he’d been talking with and who knew him instantly denied they had any knowledge of him, his assault or his whereabouts. I could tell what kind of night this was going to be...
A 55 year-old Scot fell down drunk on the pavement at a bus stop and the good people standing around called an ambulance. We arrived and he was shocked at the fuss being caused. You see, where he and I come from, calling an ambulance is almost unheard of unless your head is falling off – and his wasn’t; he had a minor bruise to the side of it. Nevertheless, as he sat in the back of the car protesting his detention, we found his pulse to be a little too slow for his age (and it was irregular) and his blood pressure a little too high for his own good. So, with a good deal of repetitive arguing to and fro, we took him to hospital for an ECG. My suspicion was heart block but he could easily just have fallen down as a result of his inebriated state – he certainly wasn’t steady on his feet at all but the risk was also high that he didn’t just happen to have a slow, irregular pulse and high blood pressure as part of his design.
He was pleasant enough, in-between the odd profanity, which he denied spitting out when I asked him to refrain and my Glaswegian helped break the ice when our accents and colloquialisms collided.
Later on we were asked to go to an assault scene to check the welfare of the crew that had been assigned, as they’re vehicle was still showing on scene but nobody had called in to update Control, so there was concern about what may have happened to them. When we got there, outside a closed pub, there was no sign of an ambulance. This was a good thing because it meant the system had gone awry and not the crew, who’d obviously cleared the area and either taken the patient to hospital or left her alone and gone home after their shift.
The second assault of the night had us running south to a dodgy estate where an even dodgier flat contained a dodgy drug-user/dealer. He had a minor head injury and the police had been called by a neighbour who’d heard a disturbance earlier and then ‘some men’ had been seen scuttling away from the premises. I had a quick look around the place while the student did the obs and chatted with the 60 year-old Liverpudlian about what had happened. He said he had no recollection of being hit but that somebody had stolen his stash of drugs.
His injury had been caused by a narrow, pointed weapon and I noticed that he was sitting on a nasty looking crow-bar. This was probably what did the damage. He’d had a disagreement with his lugubrious druggy mates and during the inevitable scuffle he’d probably been smacked in the face with his own weapon. He’d started to become aggressive and verbally abusive towards us all now anyway and me noticing the iron bar had at least made it possible for one of the officers to remove it and make him less of an immediate danger to us. ‘I want you people to leave’ he said. It took less than a second for me to agree with him and do as we were told. I am not going to get injured doing this job if I can help it and neither am I going to be responsible for any injury done to someone in my charge.
As the early hours became late early we were sent to an 84 year-old lady with a nose bleed. She had suffered a stroke a few years ago and was bed-bound with hemiplegia. Her partner in the cramped little flat suffered COPD and was on an oxygen lifeline and it was almost sadly comical to watch when he shuffled in to her bedroom as we checked her over; he gasped and wheezed his way to the chair and began to chat about how much he worried about his friend. I was worrying more about him now.
The patient seemed back to normal after her fright – she’d woken up with blood in her mouth and her nose was pouring blood out onto the sheets. A few heavy dark clots sat around her and we cleaned her up as best we could. Her top had to be changed but after a half hour of wiping away red stains from her chin, neck and face, she was fine again.
Both of them had a wicked sense of humour and I exploited that to help me adjust my decision making because I initially wanted to leave her at home, where she was happier, and get a doctor to come and see them both to ensure they were okay but as we chatted and laughed I noticed that her hand was clawed in and she was trying to open it up. Her arm was paralysed but she could usually open the hand – now she couldn’t, so there was a change in her that needed further investigating. I asked for an ambulance and a crew arrived within ten minutes to take her to hospital. Given her history and this recent change, notwithstanding that sudden nosebleed, it was no longer safe to leave her at home, even in the care of her friend. I also organised a doctor to visit her partner because his breathing needed to be stabilised.
This couple have been living like this for years; both of them are quite ill but both have reached a good age and have no bitterness or regrets. They laughed and joked their way through our visit with them and we spoke about ‘getting on with it’ even though things aren’t great. I have the greatest respect for them. We deal with many younger people, in better circumstances, who have no sense of fortune and who cannot see that their fate is ultimately designed by themselves.
Be safe.
Stats: 2 Assaults; 1 eTOH; 1 Epistaxis.
I have a couple of nights with my student paramedic on board and before we’d even got a proper job, a man ran at the car in Soho and complained that he’d been assaulted and that we should treat him and call the police. He was a bit wild-eyed and edgy, so I called for police and watched as my student attempted to deal with his childishly minor injury, caused by a punch to the mouth. He got predictably annoying and aggressive and so I asked him to go and that the police would deal with it.
By the time the cops arrived on foot he’d long gone and the people he’d been talking with and who knew him instantly denied they had any knowledge of him, his assault or his whereabouts. I could tell what kind of night this was going to be...
A 55 year-old Scot fell down drunk on the pavement at a bus stop and the good people standing around called an ambulance. We arrived and he was shocked at the fuss being caused. You see, where he and I come from, calling an ambulance is almost unheard of unless your head is falling off – and his wasn’t; he had a minor bruise to the side of it. Nevertheless, as he sat in the back of the car protesting his detention, we found his pulse to be a little too slow for his age (and it was irregular) and his blood pressure a little too high for his own good. So, with a good deal of repetitive arguing to and fro, we took him to hospital for an ECG. My suspicion was heart block but he could easily just have fallen down as a result of his inebriated state – he certainly wasn’t steady on his feet at all but the risk was also high that he didn’t just happen to have a slow, irregular pulse and high blood pressure as part of his design.
He was pleasant enough, in-between the odd profanity, which he denied spitting out when I asked him to refrain and my Glaswegian helped break the ice when our accents and colloquialisms collided.
Later on we were asked to go to an assault scene to check the welfare of the crew that had been assigned, as they’re vehicle was still showing on scene but nobody had called in to update Control, so there was concern about what may have happened to them. When we got there, outside a closed pub, there was no sign of an ambulance. This was a good thing because it meant the system had gone awry and not the crew, who’d obviously cleared the area and either taken the patient to hospital or left her alone and gone home after their shift.
The second assault of the night had us running south to a dodgy estate where an even dodgier flat contained a dodgy drug-user/dealer. He had a minor head injury and the police had been called by a neighbour who’d heard a disturbance earlier and then ‘some men’ had been seen scuttling away from the premises. I had a quick look around the place while the student did the obs and chatted with the 60 year-old Liverpudlian about what had happened. He said he had no recollection of being hit but that somebody had stolen his stash of drugs.
His injury had been caused by a narrow, pointed weapon and I noticed that he was sitting on a nasty looking crow-bar. This was probably what did the damage. He’d had a disagreement with his lugubrious druggy mates and during the inevitable scuffle he’d probably been smacked in the face with his own weapon. He’d started to become aggressive and verbally abusive towards us all now anyway and me noticing the iron bar had at least made it possible for one of the officers to remove it and make him less of an immediate danger to us. ‘I want you people to leave’ he said. It took less than a second for me to agree with him and do as we were told. I am not going to get injured doing this job if I can help it and neither am I going to be responsible for any injury done to someone in my charge.
As the early hours became late early we were sent to an 84 year-old lady with a nose bleed. She had suffered a stroke a few years ago and was bed-bound with hemiplegia. Her partner in the cramped little flat suffered COPD and was on an oxygen lifeline and it was almost sadly comical to watch when he shuffled in to her bedroom as we checked her over; he gasped and wheezed his way to the chair and began to chat about how much he worried about his friend. I was worrying more about him now.
The patient seemed back to normal after her fright – she’d woken up with blood in her mouth and her nose was pouring blood out onto the sheets. A few heavy dark clots sat around her and we cleaned her up as best we could. Her top had to be changed but after a half hour of wiping away red stains from her chin, neck and face, she was fine again.
Both of them had a wicked sense of humour and I exploited that to help me adjust my decision making because I initially wanted to leave her at home, where she was happier, and get a doctor to come and see them both to ensure they were okay but as we chatted and laughed I noticed that her hand was clawed in and she was trying to open it up. Her arm was paralysed but she could usually open the hand – now she couldn’t, so there was a change in her that needed further investigating. I asked for an ambulance and a crew arrived within ten minutes to take her to hospital. Given her history and this recent change, notwithstanding that sudden nosebleed, it was no longer safe to leave her at home, even in the care of her friend. I also organised a doctor to visit her partner because his breathing needed to be stabilised.
This couple have been living like this for years; both of them are quite ill but both have reached a good age and have no bitterness or regrets. They laughed and joked their way through our visit with them and we spoke about ‘getting on with it’ even though things aren’t great. I have the greatest respect for them. We deal with many younger people, in better circumstances, who have no sense of fortune and who cannot see that their fate is ultimately designed by themselves.
Be safe.
Friday 5 February 2010
Assault
Day shift: Five calls; two by car; three by ambulance.
Stats: 1 Epistaxis; 2 Chest pain;1 Collapsed person; 1 Assault.
An epistaxis at the start of the shift and with no ambulance available in support. Most of these turn out to be little trickles of nothingness or are under control by the time I get on scene but this one, at a hotel/hostel, was different. The 55 year-old alcoholic and drug addict had been suffering 30-minute nosebleeds for the past few days but had been dealing with them himself. This morning, however, he became more concerned when yet another nosebleed struck and couldn’t be stopped.
When I arrived he’d already been bleeding for half an hour and he was holding a blood-soaked bar towel to his nose. The flow was watery and constant – not a clot in sight – and he admitted to having taken heroin and cocaine (brown and white) the day before, as well as drinking alcohol but he didn’t snort the coke, so there was probably another, possibly unrelated reason for this flood of blood.
I put a heavy dressing on the nose and wrapped it around his head but the blood just soaked through it, so I put another on after I’d done his basic obs and made it a little tighter – this seemed to work. Then I got him in the car and took him quickly to hospital. No ambulances had been assigned and there was nothing on the horizon. I wasn’t prepared to sit there while he bled and bled, so I took him myself without a hitch or a complaint.
After a morning meeting and a quick run to help out with a regular caller who feigns chest pain for a hospital bed (a call on which I was no use at all because an ambulance had been sent) I went to the aid of a 39 year-old nurse who was complaining of chest pain with shortness of breath (SOB). This had been going on, minus the SOB, for a year and she’d been ignoring it as it always got better but now that her breathing was being affected she felt it best to get checked out, as she should. All her obs were normal and her ECG shouted out nothing of any consequence that I could see but something was amiss and her SOB was related, so she was taken by ambulance to hospital.
A Red call for a collapsed ‘unconscious’ woman resulted in myself and a crew arriving at the same time and climbing lots of narrow little steps to a flat at the top of a building in Soho. She wasn’t unconscious but her husband was dramatically bent over her starfish body as her eyelids fluttered (the tell-tale sign of someone who wants to be unconscious but actually isn’t). She has been suffering from post-natal depression and this was not her first dramatic collapse. She needs further medical care I feel because she isn’t getting better. I’m not unsympathetic here though because PND is a very real and significant problem and she wasn’t coping well with it, so her husband was being left literally ‘holding the baby’. We can do nothing for her and the support she gets from her own is really crucial.
Racism and the general hatred of uniforms and authority of any kind is on the rise in my opinion, regardless of the soap the statistics are being washed with by the Government. A 30 year-old Iranian Traffic Enforcer (Warden?) was allegedly assaulted by two men who chased him, challenging him to a fight and hurling verbal abuse, including some nasty racist comments after he’d issued a ticket. They allegedly grabbed him and used his own ticketing machine to thump him in the chest, right where he’d broken a rib earlier in his life. Now he had sharp pain which was worse when he breathed in deeply.
None of us like getting tickets and parking fines but it’s the system and costs we dislike, not the people doing the job, although most react as if it is personal. A lot of these enforcers will actually be lenient with you and give you a bit of a break if your reaction to them is positive. If they don’t, that’s tough and we all have to pay the fines if they are valid. What we can’t do is assault them for doing the job. And as for racist taunts about not being in this country and taking jobs from Brits, well, where are these Brits? Clearly, they don’t want to do those jobs. This man is in the country, working hard and paying taxes – contributing to society, like it or not. He's not leeching from the State or causing trouble.
We chatted about his country’s current predicament, given that there are practically unveiled threats to attack it and he said ‘why does everyone hate us’ - the man was genuinely distressed about what had happened to him. That’s the problem with the media – they report the ‘evil axis’ stuff and yes, there may be a problem developing in terms of possible nuclear weapons but haven’t we heard all this before? And Iranian people should not be demonised as a population just because of the bad apples. You don't see them falling about drunk in the street and you will rarely, if ever meet an Iranian who is disrespectful. The meat and two veg of my repeated complaints about what is happening to our society is relative to everyone who behaves badly and shouldn't - nothing whatsoever to do with who they are or where they come from because we Brits can often be the worst examples of how to live as a society.
I'm only five foot seven, so I needed a box to stand on for that. Phew!
Be safe.
Stats: 1 Epistaxis; 2 Chest pain;1 Collapsed person; 1 Assault.
An epistaxis at the start of the shift and with no ambulance available in support. Most of these turn out to be little trickles of nothingness or are under control by the time I get on scene but this one, at a hotel/hostel, was different. The 55 year-old alcoholic and drug addict had been suffering 30-minute nosebleeds for the past few days but had been dealing with them himself. This morning, however, he became more concerned when yet another nosebleed struck and couldn’t be stopped.
When I arrived he’d already been bleeding for half an hour and he was holding a blood-soaked bar towel to his nose. The flow was watery and constant – not a clot in sight – and he admitted to having taken heroin and cocaine (brown and white) the day before, as well as drinking alcohol but he didn’t snort the coke, so there was probably another, possibly unrelated reason for this flood of blood.
I put a heavy dressing on the nose and wrapped it around his head but the blood just soaked through it, so I put another on after I’d done his basic obs and made it a little tighter – this seemed to work. Then I got him in the car and took him quickly to hospital. No ambulances had been assigned and there was nothing on the horizon. I wasn’t prepared to sit there while he bled and bled, so I took him myself without a hitch or a complaint.
After a morning meeting and a quick run to help out with a regular caller who feigns chest pain for a hospital bed (a call on which I was no use at all because an ambulance had been sent) I went to the aid of a 39 year-old nurse who was complaining of chest pain with shortness of breath (SOB). This had been going on, minus the SOB, for a year and she’d been ignoring it as it always got better but now that her breathing was being affected she felt it best to get checked out, as she should. All her obs were normal and her ECG shouted out nothing of any consequence that I could see but something was amiss and her SOB was related, so she was taken by ambulance to hospital.
A Red call for a collapsed ‘unconscious’ woman resulted in myself and a crew arriving at the same time and climbing lots of narrow little steps to a flat at the top of a building in Soho. She wasn’t unconscious but her husband was dramatically bent over her starfish body as her eyelids fluttered (the tell-tale sign of someone who wants to be unconscious but actually isn’t). She has been suffering from post-natal depression and this was not her first dramatic collapse. She needs further medical care I feel because she isn’t getting better. I’m not unsympathetic here though because PND is a very real and significant problem and she wasn’t coping well with it, so her husband was being left literally ‘holding the baby’. We can do nothing for her and the support she gets from her own is really crucial.
Racism and the general hatred of uniforms and authority of any kind is on the rise in my opinion, regardless of the soap the statistics are being washed with by the Government. A 30 year-old Iranian Traffic Enforcer (Warden?) was allegedly assaulted by two men who chased him, challenging him to a fight and hurling verbal abuse, including some nasty racist comments after he’d issued a ticket. They allegedly grabbed him and used his own ticketing machine to thump him in the chest, right where he’d broken a rib earlier in his life. Now he had sharp pain which was worse when he breathed in deeply.
None of us like getting tickets and parking fines but it’s the system and costs we dislike, not the people doing the job, although most react as if it is personal. A lot of these enforcers will actually be lenient with you and give you a bit of a break if your reaction to them is positive. If they don’t, that’s tough and we all have to pay the fines if they are valid. What we can’t do is assault them for doing the job. And as for racist taunts about not being in this country and taking jobs from Brits, well, where are these Brits? Clearly, they don’t want to do those jobs. This man is in the country, working hard and paying taxes – contributing to society, like it or not. He's not leeching from the State or causing trouble.
We chatted about his country’s current predicament, given that there are practically unveiled threats to attack it and he said ‘why does everyone hate us’ - the man was genuinely distressed about what had happened to him. That’s the problem with the media – they report the ‘evil axis’ stuff and yes, there may be a problem developing in terms of possible nuclear weapons but haven’t we heard all this before? And Iranian people should not be demonised as a population just because of the bad apples. You don't see them falling about drunk in the street and you will rarely, if ever meet an Iranian who is disrespectful. The meat and two veg of my repeated complaints about what is happening to our society is relative to everyone who behaves badly and shouldn't - nothing whatsoever to do with who they are or where they come from because we Brits can often be the worst examples of how to live as a society.
I'm only five foot seven, so I needed a box to stand on for that. Phew!
Be safe.
Thursday 4 February 2010
Saying it like it is
Day shift: Five calls; one assisted-only; one by ambulance; three by car.
Stats: 1 Feeling weak; 1 Abdo pain; 1 Period pain; 1 Shoulder injury; 1 eTOH.
A 65 year-old man with advancing Alzheimer’s found himself unable to stand due to weakness and his carer on scene told me of his recent UTI and vascular problems, none of which were likely culprits. He wasn’t eating or drinking fluids well, so I suspect he may have had an electrolyte imbalance and his ECG, despite him having a pacemaker fitted, was throwing off PVC’s with a resulting bradycardia and pulse irregularity. He was taken to hospital for treatment and to have the pacemaker checked.
Following on after a pause, a 21 year-old at college felt the need to roll around the floor and ‘pass in and out of consciousness’ as he experienced abdominal pain that was probably brought on by constipation. He hadn’t opened his bowels for a while (in fact he couldn’t remember the last time but then again, he couldn’t remember his address when I asked him) and he had no medical problems, past or present. He continued to roll about a bit when security had shown me to where he’d been deposited but his ‘passing out’ phase had ended, thank goodness.
Until this call, the one I’m about to relate, I thought I was in for a day of wasted reasons to drive anywhere in a hurry. The call was for a 28 year-old female who had severe period pains / food poisoning, an anomaly that was explained to me later on by the patient. So, I walked into the store where the call had originated (a place I’ve visited many times and who seem hell bent on calling 999 every time they have the most minor of problems) and was taken, after a long delay while they tried to find someone to guide me, to the basement rabbit run and then the first aid room where my patient lay, somewhat embarrassed, on a couch. ‘Don’t worry, I think its only period pain’, she said after describing her dizziness and vomiting and abdo pain. This was normal for her on the first day of her period and she’d asked the management of the store not to call an ambulance but they’d insisted. In fact, when she’d asked for a hot water bottle, which she knew would help (filled with hot water obviously), they refused to get her one – even though she’d offered to pay for it. She'd mentiond food poisoning as a possibility but ruled it out but panic set in with the manager I think.
This was a thoroughly sensible young lady who knew that a trip to A&E for her problem would be an exaggeration of need, so I did a full set of obs, found her to be normal, alive and well then made a pact with her to sign my PRF and take a copy away in case she needed urgent medical help. She wouldn’t be going to hospital and she smiled acknowledgment to sense. Then, as she should in order to therapeutically resolve her current issue, she went back to continue shopping.
During this call, I was sent another and went west to transport a patient of one of our cycle buddies. The man, a 55 year-old Englishman now residing in South Africa with his wife, fell down a few steps in a shop, landing on his arm and damaging his shoulder. He could bend his arm but he could not lift it, indicating a problem with the joint at the shoulder itself.
I had a long and very interesting conversation with them both as they travelled to hospital with me. We talked about South Africa, how dangerous it could be and how beautiful it was. We touched on all kinds of politics, some of which would be angrily protested by anyone with a mind that was closed to free thought. It was refreshing to speak my mind and hear others do so too. Actually, just typing that statement is a damning indictment on the current state of free speech in this country.
Freedom, while we are on the subject, also allows alcoholic East European gentlemen to come to the UK and lie on the pavement (conveniently outside a pub), thrashing around pretending to have an epileptic fit when, (and the proof was there), it was patently obvious that he just wanted an excuse to be conveyed to a hospital. In fact, in between ‘fits’ he was able to make demands and one of them was that he wanted to go to a specific hospital. Believe me, I would be just as harsh about this behaviour if it was a fellow Scot but we are actually importing this nonsense and to concern ourselves about it is to risk being dubbed ‘racist’ by some. It’s not of course; it’s about being blindsided and stupid enough to fall for it in a country where liberal leniency has gone off the deep end and where, no doubt, it wouldn’t be tolerated quite as much in its country of origin.
So, I knew him because he’s done this before, many times. There are people with genuine epilepsy who would not appreciate his efforts at replicating it. His burden on you and me is financial at a time when we are seriously worried about funding cuts for schools, hospitals and universities. Yet he is given money to go and get drunk then when he runs out of booze he pretends to be ill, goes to hospital and, no doubt, attempts to find the means to substitute it for something else drinkable. He does this while chucking verbal abuse at us all.
He attempted to smoke several times in the car as I took him, with an accompanying police officer, to hospital. Then he tried it again as he waited to be seen by a nurse. They all knew him but nothing will be done about him because we have no solution that satisfies everyone – like when I write this stuff; someone, somewhere will always take offence, either because they think I’m saying all East Europeans are like this, which I am not or that I am saying all alcoholics are like this – which I am not. I’m trying out my freedom of speech thing to see if it flies.
And he said something profoundly ironic in the car as he argued with the cop, ‘I drink but I don’t take drugs’.
Be safe.
Stats: 1 Feeling weak; 1 Abdo pain; 1 Period pain; 1 Shoulder injury; 1 eTOH.
A 65 year-old man with advancing Alzheimer’s found himself unable to stand due to weakness and his carer on scene told me of his recent UTI and vascular problems, none of which were likely culprits. He wasn’t eating or drinking fluids well, so I suspect he may have had an electrolyte imbalance and his ECG, despite him having a pacemaker fitted, was throwing off PVC’s with a resulting bradycardia and pulse irregularity. He was taken to hospital for treatment and to have the pacemaker checked.
Following on after a pause, a 21 year-old at college felt the need to roll around the floor and ‘pass in and out of consciousness’ as he experienced abdominal pain that was probably brought on by constipation. He hadn’t opened his bowels for a while (in fact he couldn’t remember the last time but then again, he couldn’t remember his address when I asked him) and he had no medical problems, past or present. He continued to roll about a bit when security had shown me to where he’d been deposited but his ‘passing out’ phase had ended, thank goodness.
Until this call, the one I’m about to relate, I thought I was in for a day of wasted reasons to drive anywhere in a hurry. The call was for a 28 year-old female who had severe period pains / food poisoning, an anomaly that was explained to me later on by the patient. So, I walked into the store where the call had originated (a place I’ve visited many times and who seem hell bent on calling 999 every time they have the most minor of problems) and was taken, after a long delay while they tried to find someone to guide me, to the basement rabbit run and then the first aid room where my patient lay, somewhat embarrassed, on a couch. ‘Don’t worry, I think its only period pain’, she said after describing her dizziness and vomiting and abdo pain. This was normal for her on the first day of her period and she’d asked the management of the store not to call an ambulance but they’d insisted. In fact, when she’d asked for a hot water bottle, which she knew would help (filled with hot water obviously), they refused to get her one – even though she’d offered to pay for it. She'd mentiond food poisoning as a possibility but ruled it out but panic set in with the manager I think.
This was a thoroughly sensible young lady who knew that a trip to A&E for her problem would be an exaggeration of need, so I did a full set of obs, found her to be normal, alive and well then made a pact with her to sign my PRF and take a copy away in case she needed urgent medical help. She wouldn’t be going to hospital and she smiled acknowledgment to sense. Then, as she should in order to therapeutically resolve her current issue, she went back to continue shopping.
During this call, I was sent another and went west to transport a patient of one of our cycle buddies. The man, a 55 year-old Englishman now residing in South Africa with his wife, fell down a few steps in a shop, landing on his arm and damaging his shoulder. He could bend his arm but he could not lift it, indicating a problem with the joint at the shoulder itself.
I had a long and very interesting conversation with them both as they travelled to hospital with me. We talked about South Africa, how dangerous it could be and how beautiful it was. We touched on all kinds of politics, some of which would be angrily protested by anyone with a mind that was closed to free thought. It was refreshing to speak my mind and hear others do so too. Actually, just typing that statement is a damning indictment on the current state of free speech in this country.
Freedom, while we are on the subject, also allows alcoholic East European gentlemen to come to the UK and lie on the pavement (conveniently outside a pub), thrashing around pretending to have an epileptic fit when, (and the proof was there), it was patently obvious that he just wanted an excuse to be conveyed to a hospital. In fact, in between ‘fits’ he was able to make demands and one of them was that he wanted to go to a specific hospital. Believe me, I would be just as harsh about this behaviour if it was a fellow Scot but we are actually importing this nonsense and to concern ourselves about it is to risk being dubbed ‘racist’ by some. It’s not of course; it’s about being blindsided and stupid enough to fall for it in a country where liberal leniency has gone off the deep end and where, no doubt, it wouldn’t be tolerated quite as much in its country of origin.
So, I knew him because he’s done this before, many times. There are people with genuine epilepsy who would not appreciate his efforts at replicating it. His burden on you and me is financial at a time when we are seriously worried about funding cuts for schools, hospitals and universities. Yet he is given money to go and get drunk then when he runs out of booze he pretends to be ill, goes to hospital and, no doubt, attempts to find the means to substitute it for something else drinkable. He does this while chucking verbal abuse at us all.
He attempted to smoke several times in the car as I took him, with an accompanying police officer, to hospital. Then he tried it again as he waited to be seen by a nurse. They all knew him but nothing will be done about him because we have no solution that satisfies everyone – like when I write this stuff; someone, somewhere will always take offence, either because they think I’m saying all East Europeans are like this, which I am not or that I am saying all alcoholics are like this – which I am not. I’m trying out my freedom of speech thing to see if it flies.
And he said something profoundly ironic in the car as he argued with the cop, ‘I drink but I don’t take drugs’.
Be safe.
Wednesday 3 February 2010
Hop it
Day shift: Five calls; one treated on scene; two by ambulance; two by car.
Stats: 1 Feeling faint; 1 ? Fractured Humerus; 1 Sprained ankle; 1 TIA; 1 Epistaxis.
I started the day with a ‘feeling faint’ that may or may not have had more to do with stress than the assumed cardiac connection made and given a resultant Red category. The 56 year-old man was at work in an office and has had two days of feeling like he was ‘missing a breath and a heartbeat’ every now and then. He also felt dizzy and faint and had visual disturbances at times, especially when he was sitting in front of his computer for any length of time concentrating.
He was taking beta blockers for diagnosed high blood pressure and when I checked it I found it to be up there at 180/90, so this gave the call a non-routine complexion but, before we all dive off the deep end, he looked stressed. He looked like he was the stressy type and he admitted to being so. He also knew what white coat syndrome was and so his blood pressure would probably have been behaving according to his disposition at the time. I will doubtless hear the ‘but his beta blockers would surely have been controlling that’ argument but I’ve seen this a lot and stress is a major factor for such changes in non-critical circumstances. His visual problems and that feeling of missing a breath could be down to anxiety. Nevertheless, he needed an ECG (incidentally, he had no chest pain) and a more thorough check up before a conclusion based on his lifestyle could be determined. If I was able to describe this man and then the environment in which he worked, you’d understand my reluctance to worry too much about him.
Then an 84 year-old lady stumbled over a quite frankly stupid and impractical device, comprising a length of rope and a few metal posts at ankle height, designed to prevent people from getting to close to works of art (paintings) at a gallery. She fell onto her knees and then slammed into the wall below the painting, damaging and probably fracturing, her mid-shaft humerus. This is a painful and significant injury at any age, never mind mid-80’s.
Luckily she was the strong type and, apart from the arm injury, had sustained no other damage on her trip. There was no first aid room or anywhere suitable to take her for obs and conversation about her personal medical history (this is, as you know, a real bug for me) and so, with the help of security and her friends, we wheeled her to the best place we could find for this – a conference room in which a small meeting was taking place. People were cleared and apologised to but I think this elderly lady will be writing harsh words about the stupidity of that small barrier (what’s it for, nosey dogs?) and the lack of proper facilities in a crowded place.
Sprained ankles are not generally life threatening, so if you are 28 years-old and can hop, either get a taxi or a friend to take you to the nearest A&E or Minor Injuries Unit where you will wait for possibly hours as they wheel in one true emergency after another. This man, who was on his way to work when he slipped on steps and twisted his ankle, continued on until he could no longer put weight on it before allowing his colleagues to dial 999 and declare it an emergency. There was no first aider to be seen, even though in a company that large there should have been and he had been given no treatment for it. His shoe and sock were still on his affected foot. A smart first aider would have assessed it, seen it for what it was (a sprain), given it the old RICE treatment and then had him taken to hospital for an x-ray, if required (and under the Ottowa rules it probably was) and that would have been the end of it. That being done, someone dying in the street elsewhere would get a timely ambulance response in the hope that the dying thing could be reversed.
At one of the nicest hotels in London a 65 year-old American woman had a small stroke – a TIA – whilst having her hair done. One of the other FRU’s on duty was called first and I got there a few seconds behind in support because the initial call sounded like it was going to become a suspended (cardiac arrest).
The woman had been put in the recovery position by a member of staff and she was completely unaware and unable to communicate. One side was weak and she was mildly combative when things were done to her, such as the BM check but oxygen helped her to recover and she went from incapable to survivor in ten minutes. She was able to speak a little when we started to move her down to the ambulance, where her frail and elderly husband waited in the street, hotel staff members all around him.
The lady’s ECG showed PVC’s after every normal beat, running in pairs – known as bigeminal couplets; something we don’t get to see much of, so it was interesting to analyse. She was taken, with her husband, to hospital on blue lights and the hotel manager promised a car would pick one or both of them up and return them to their room, depending on the outcome, which is hopefully favourable.
In a cruel twist they sent me to women-only spa where a 45 year-old lady was having a nosebleed that had gone on for 30 minutes. So, I was chaperoned all the way through to the changing rooms and had to stand in a small toilet with the lady and her friend as I covered her poorly nose until it stopped bleeding and we could all put it behind us. Actually, she was the sensible type and had experienced these epistaxal experiences before; they always occurred after having a cold and then going into warm places (like a spa for example). This was her longest bleed though, so her friend got panicky and made the patient feel embarrassed when I walked in to help her with something she’d been able to deal with all her adult life. I made things better for her by assuring her that she didn’t have to go to A&E if she didn’t want to, (which she didn’t) and that HEMS were being stood down.
Then I went home.
Be safe.
Stats: 1 Feeling faint; 1 ? Fractured Humerus; 1 Sprained ankle; 1 TIA; 1 Epistaxis.
I started the day with a ‘feeling faint’ that may or may not have had more to do with stress than the assumed cardiac connection made and given a resultant Red category. The 56 year-old man was at work in an office and has had two days of feeling like he was ‘missing a breath and a heartbeat’ every now and then. He also felt dizzy and faint and had visual disturbances at times, especially when he was sitting in front of his computer for any length of time concentrating.
He was taking beta blockers for diagnosed high blood pressure and when I checked it I found it to be up there at 180/90, so this gave the call a non-routine complexion but, before we all dive off the deep end, he looked stressed. He looked like he was the stressy type and he admitted to being so. He also knew what white coat syndrome was and so his blood pressure would probably have been behaving according to his disposition at the time. I will doubtless hear the ‘but his beta blockers would surely have been controlling that’ argument but I’ve seen this a lot and stress is a major factor for such changes in non-critical circumstances. His visual problems and that feeling of missing a breath could be down to anxiety. Nevertheless, he needed an ECG (incidentally, he had no chest pain) and a more thorough check up before a conclusion based on his lifestyle could be determined. If I was able to describe this man and then the environment in which he worked, you’d understand my reluctance to worry too much about him.
Then an 84 year-old lady stumbled over a quite frankly stupid and impractical device, comprising a length of rope and a few metal posts at ankle height, designed to prevent people from getting to close to works of art (paintings) at a gallery. She fell onto her knees and then slammed into the wall below the painting, damaging and probably fracturing, her mid-shaft humerus. This is a painful and significant injury at any age, never mind mid-80’s.
Luckily she was the strong type and, apart from the arm injury, had sustained no other damage on her trip. There was no first aid room or anywhere suitable to take her for obs and conversation about her personal medical history (this is, as you know, a real bug for me) and so, with the help of security and her friends, we wheeled her to the best place we could find for this – a conference room in which a small meeting was taking place. People were cleared and apologised to but I think this elderly lady will be writing harsh words about the stupidity of that small barrier (what’s it for, nosey dogs?) and the lack of proper facilities in a crowded place.
Sprained ankles are not generally life threatening, so if you are 28 years-old and can hop, either get a taxi or a friend to take you to the nearest A&E or Minor Injuries Unit where you will wait for possibly hours as they wheel in one true emergency after another. This man, who was on his way to work when he slipped on steps and twisted his ankle, continued on until he could no longer put weight on it before allowing his colleagues to dial 999 and declare it an emergency. There was no first aider to be seen, even though in a company that large there should have been and he had been given no treatment for it. His shoe and sock were still on his affected foot. A smart first aider would have assessed it, seen it for what it was (a sprain), given it the old RICE treatment and then had him taken to hospital for an x-ray, if required (and under the Ottowa rules it probably was) and that would have been the end of it. That being done, someone dying in the street elsewhere would get a timely ambulance response in the hope that the dying thing could be reversed.
At one of the nicest hotels in London a 65 year-old American woman had a small stroke – a TIA – whilst having her hair done. One of the other FRU’s on duty was called first and I got there a few seconds behind in support because the initial call sounded like it was going to become a suspended (cardiac arrest).
The woman had been put in the recovery position by a member of staff and she was completely unaware and unable to communicate. One side was weak and she was mildly combative when things were done to her, such as the BM check but oxygen helped her to recover and she went from incapable to survivor in ten minutes. She was able to speak a little when we started to move her down to the ambulance, where her frail and elderly husband waited in the street, hotel staff members all around him.
The lady’s ECG showed PVC’s after every normal beat, running in pairs – known as bigeminal couplets; something we don’t get to see much of, so it was interesting to analyse. She was taken, with her husband, to hospital on blue lights and the hotel manager promised a car would pick one or both of them up and return them to their room, depending on the outcome, which is hopefully favourable.
In a cruel twist they sent me to women-only spa where a 45 year-old lady was having a nosebleed that had gone on for 30 minutes. So, I was chaperoned all the way through to the changing rooms and had to stand in a small toilet with the lady and her friend as I covered her poorly nose until it stopped bleeding and we could all put it behind us. Actually, she was the sensible type and had experienced these epistaxal experiences before; they always occurred after having a cold and then going into warm places (like a spa for example). This was her longest bleed though, so her friend got panicky and made the patient feel embarrassed when I walked in to help her with something she’d been able to deal with all her adult life. I made things better for her by assuring her that she didn’t have to go to A&E if she didn’t want to, (which she didn’t) and that HEMS were being stood down.
Then I went home.
Be safe.
Subscribe to:
Posts (Atom)